Left bundle branch block (LBBB) in acute myocardial infarction: the Sgarbossa criteria
Left bundle branch block (LBBB) in acute myocardial infarction (AMI): clinical implications & Sgarbossa criteria
On the contrary to right bundle branch block, left bundle branch block is always a pathological finding which affects cardiovascular and total mortality. Left bundle branch block is more common in individuals with structural and ischemic heart disease. Assessment of ischemia on ECG is difficult in the presence of left bundle branch block. This is because left bundle branch block causes substantial changes in left ventricular de- and repolarization, which result in (secondary) ST-T changes. Such ST-T changes may imitate and/or mask ischemia. Imitation of ischemia manifests as ST segment elevations in leads V1–V2 accompanied by ST segment depressions in lead V5, V6, I and aVL. Clinicians frequently confuse these elevations and depressions with those caused by STEMI (STE-ACS). Indeed, several studies have shown that the majority of patients inappropriately referred to the catheterization laboratory with suspicion of STEMI (STE-ACS) actually have left bundle branch block. Masking of ischemia occurs simply because the ST-T changes caused by the bundle branch block are stronger than the ST-T changes caused by ischemia and therefore the ischemia will not come to expression (there are exceptions to this rule, as discussed below). To overcome these difficulties, researchers have developed ECG criteria that disclose ischemia in the presence of left bundle branch block. The most successful criteria to date were developed by Elena Sgarbossa and colleagues, hence referred to as the Sgarbossa criteria.
Implications of left bundle branch block in myocardial ischemia/infarction
A summary of the issues that arise when facing a patient with left bundle branch block (LBBB) and symptoms of ischemia follow:
- Imitation: left bundle branch block causes secondary ST-T changes, with ST-segment elevations in V1–V2 and ST-segment depressions and T-wave inversions in V5, V6, aVL and I. QS complex may be seen in V1–V2.
- Masking: LBBB may mask actual ischemic ST-T changes.
- Danger: A new LBBB in patients with chest discomfort implies a relatively high probability of acute coronary artery occlusion. These patients should be managed as patients with STEMI/STE-ACS. If there are no previous ECG recordings available, one must presume that the LBBB is new.
Management of left bundle branch block (LBBB) in patients with acute coronary syndromes (ACS)
As discussed earlier, patients with chest discomfort and new or presumed new LBBB must be referred immediately to the catheterization laboratory in order to undergo angiography. This is because early studies (dating back to the 1990s) showed that patients with chest discomfort and a new (or presumed new) LBBB who were referred immediately to angiography (PCI) had better survival than comparable patients who did not undergo angiography. A significant proportion of these patients had an acute coronary artery occlusion and it was suggested that the occlusion had caused the LBBB. Ever since guidelines have recommended that patients with chest discomfort and new or presumably new LBBB should be managed as patients with STE-ACS/STEMI (i.e they should immediately undergo angiography). This will, unfortunately, lead to many unnecessary referrals because only a minority (ranging between 5% to 20%) of these patients actually have an acute occlusion. The many false positives are due to the following:
- A significant proportion of the left bundle branch blocks are not new, but simply new to the health care system (e.g lack of previous ECG recordings).
- Even if the left bundle branch block is new, the occlusion may not be total, in which case PCI does not confer any survival benefit.
Sgarbossa’s ECG criteria for detecting ischemia in the presence of left bundle branch block (LBBB)
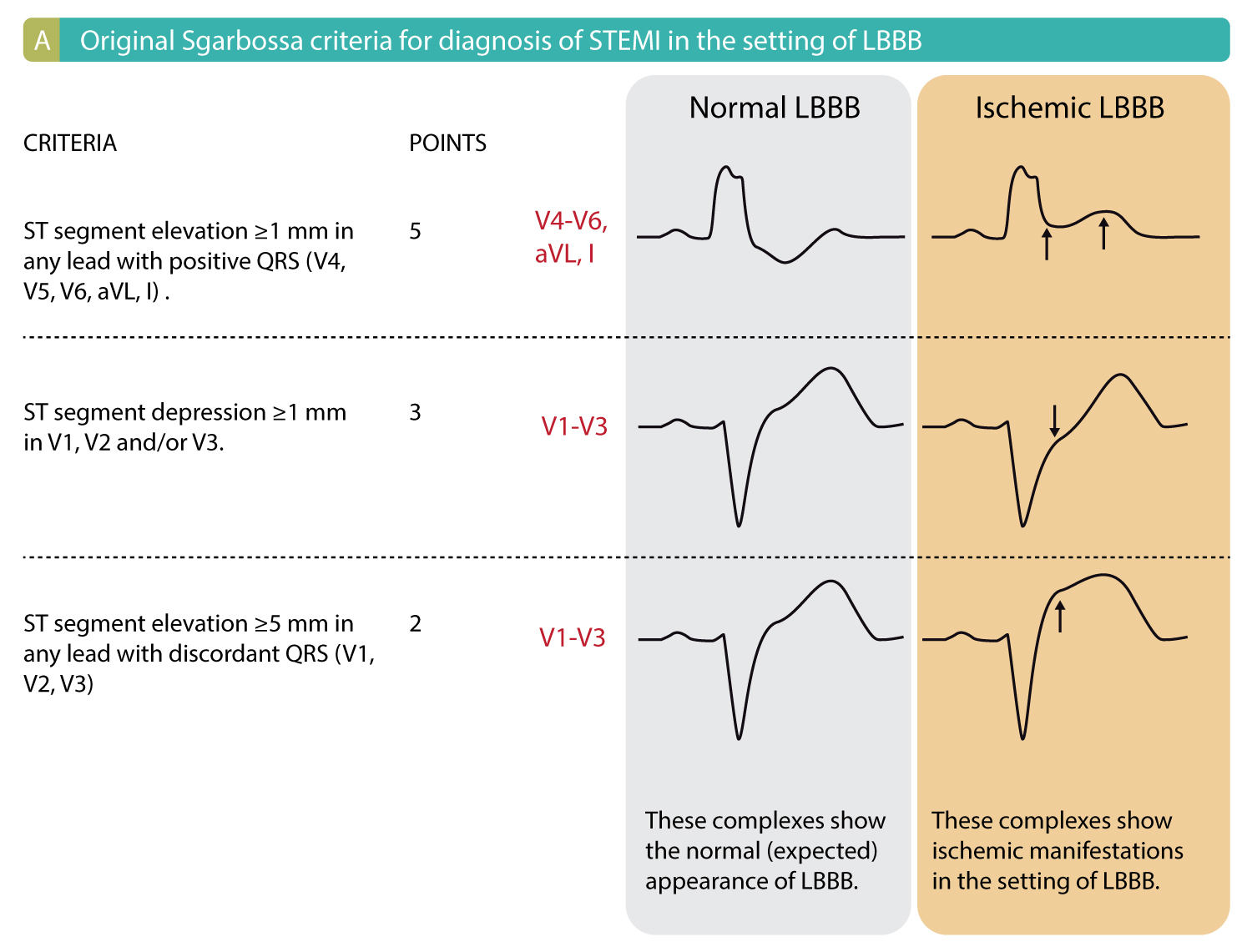
For obvious reasons, researchers have worked intensely on trying to sort out ECG changes that indicate ischemia in the presence of left bundle branch block. The greatest progress was made in 1996 by Elena Sgarbossa and colleagues (using data from the GUSTO-I study). They developed a set of criteria which are easy to use and have been validated in several studies. These criteria, referred to as Sgarbossa’s criteria, may determine whether there is acute ischemia on ECGs with LBBB. The Sgarbossa criteria consist of three simple criteria and may be applied to all left bundle branch blocks, regardless of the time of onset.
Each criterion gives 2 to 5 points. Studies show that a cut-off of ≥3 points yields a sensitivity of 20–36% and specificity of 90–98%. Figure 1A presents Sgarbossa’s criteria.
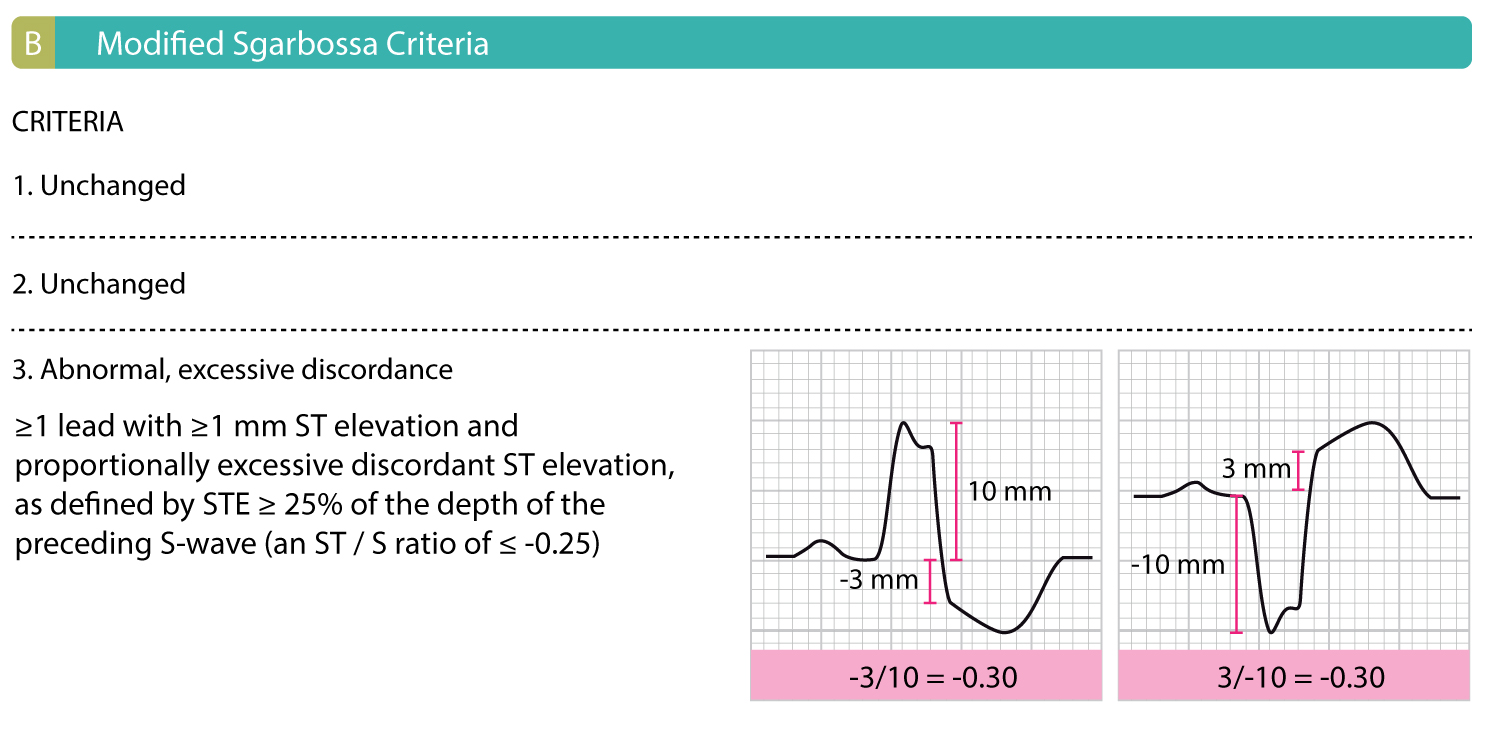
Modified Sgarbossa criteria
The modified Sgarbossa criteria, introduced by Smith et al (2012), replaces the third of the original Sgarbossa criteria (i.e the absolute 5 mm ST elevation) with an ST/S ratio less than -0.25. Measurement of the ST/S ratio is depicted in Figure 1B. Using this criterion improves the accuracy of the Sgarbossa criteria. Furthermore, the modified Sgarbossa criteria do not utilize a point system; instead, it only requires 1 of 3 criteria to be considered positive (i.e acute ischemia is strongly suggested).
Measuring ST/S ratio
Measure the amplitude of the R or S wave, whichever is most prominent, and ST segments (relative to the PR segment), to the nearest 0.5 mm. The ST/S ratio is calculated for each lead that has a discordant ST deviation of ≥1 mm. Hence, whereas the original Sgarbossa criteria utilize an absolute ST-elevation measurement, the modified criteria suggest using a rule of proportionality; the amplitude of the ST deviation is compared to the amplitude of the R or S wave, which increases both sensitivity and specificity for acute myocardial infarction.
Left bundle branch block (LBBB), left ventricular hypertrophy (LVH) and pacemaker rhythm excludes infarction criteria
European and North American guidelines assert that ECG criteria of ischemia/infarction may not be applied if the ECG shows left bundle branch block, left ventricular hypertrophy or ventricular pacemaker rhythm. This is simply because these conditions alter the ECG waveforms – both QRS and ST-T – markedly and may both mask and imitate ischemia. One is, however, free to attempt to interpret ischemia on ECGs showing these conditions. This procedure has been discussed above for left bundle branch block. Additionally, some general advice may be given (these overlap somewhat with the Sgarbossa criteria and may be applied to all three of these situations):
- Always examine if the ECG waveforms differs from earlier ECG recordings. If there are differences in the ST-T segment, it might be due to ischemia.
- Always examine if the ECG waveforms are consistent with the condition. For example, it is normal to display T-wave inversions in V5, V6, aVL and I in left bundle branch block; absence of such T-wave inversions suggest ischemia!
- Search for pseudonormalization of T-waves.
 Related chapters
Related chapters
Left Bundle Branch Block (LBBB)
Right Bundle Branch Block (RBBB)
Classification of Acute Coronary Syndromes & Myocardial Infarction: STEMI, NSTEMI & Unstable Angina
Clinical application of the ECG in chest pain and myocardial infarction
Myocardial infarction: diagnostic criteria, definitions and use of ECG
Approach to Patients with Chest Pain
ST Elevation on ECG: STEMI and Differential Diagnoses
ST depression on ECG: NSTEMI / UA and Differential Diagnoses
STEMI (ST Elevation Myocardial Infarction)
NSTEMI (Non-ST Elevation Myocardial Infarction) & Unstable Angina

