Classification of Acute Coronary Syndromes (ACS) & Acute Myocardial Infarction (AMI)
Classification, diagnosis and definitions of acute coronary syndromes (ACS) and acute myocardial infarction (AMI)
- Acute myocardial infarction: a diagnosis based on cardiac troponins
- STE-ACS (ST Elevation Acute Coronary Syndrome) & STEMI (ST Elevation Myocardial Infarction)
- NSTE-ACS (Non ST Elevation Acute Coronary Syndrome): NSTEMI (Non-ST Elevation Myocardial Infarction) & Unstable Angina
- Normalization of ECG changes
- Risk stratification in patients presenting with acute coronary syndromes: TIMI and GRACE score
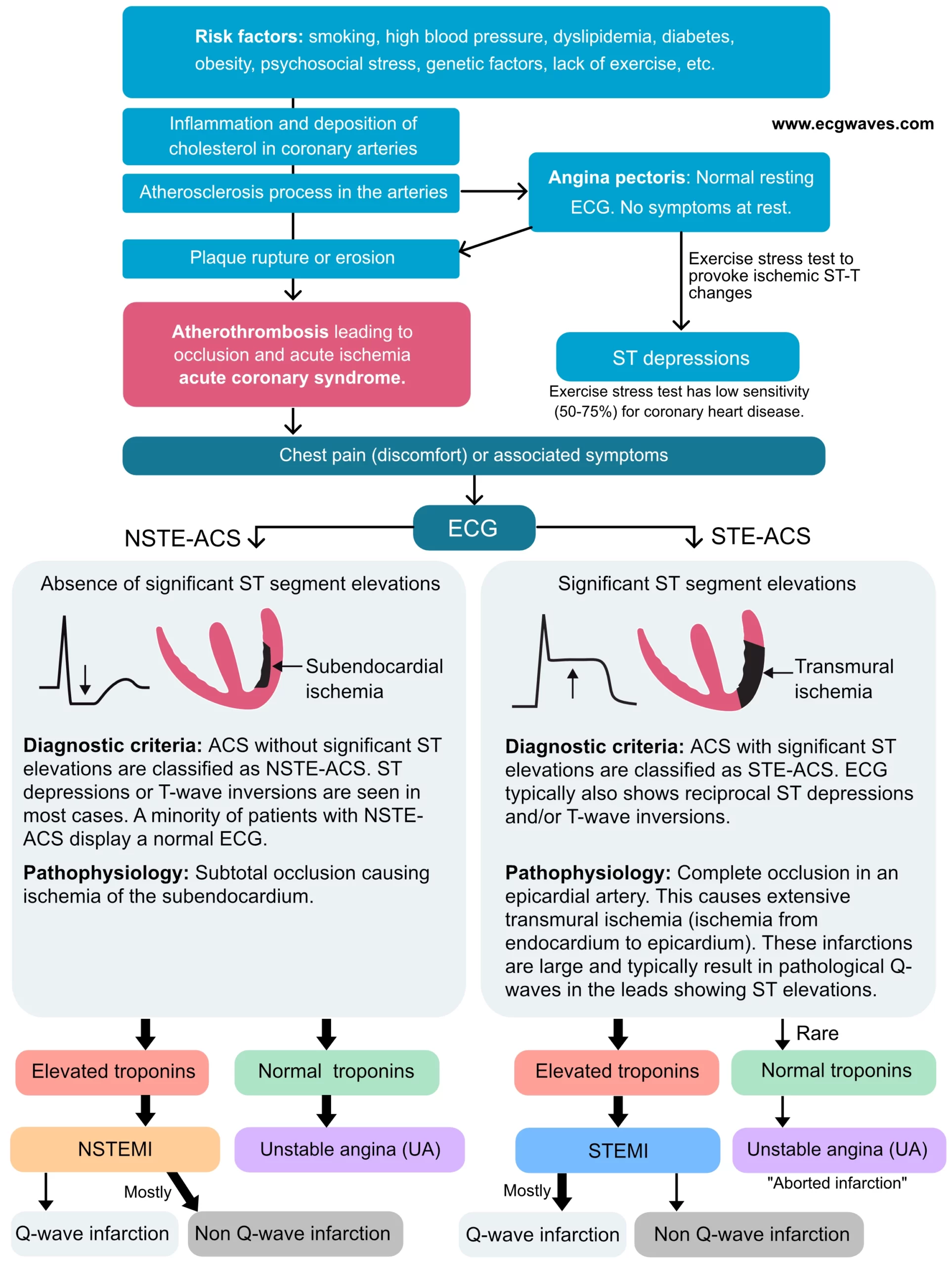
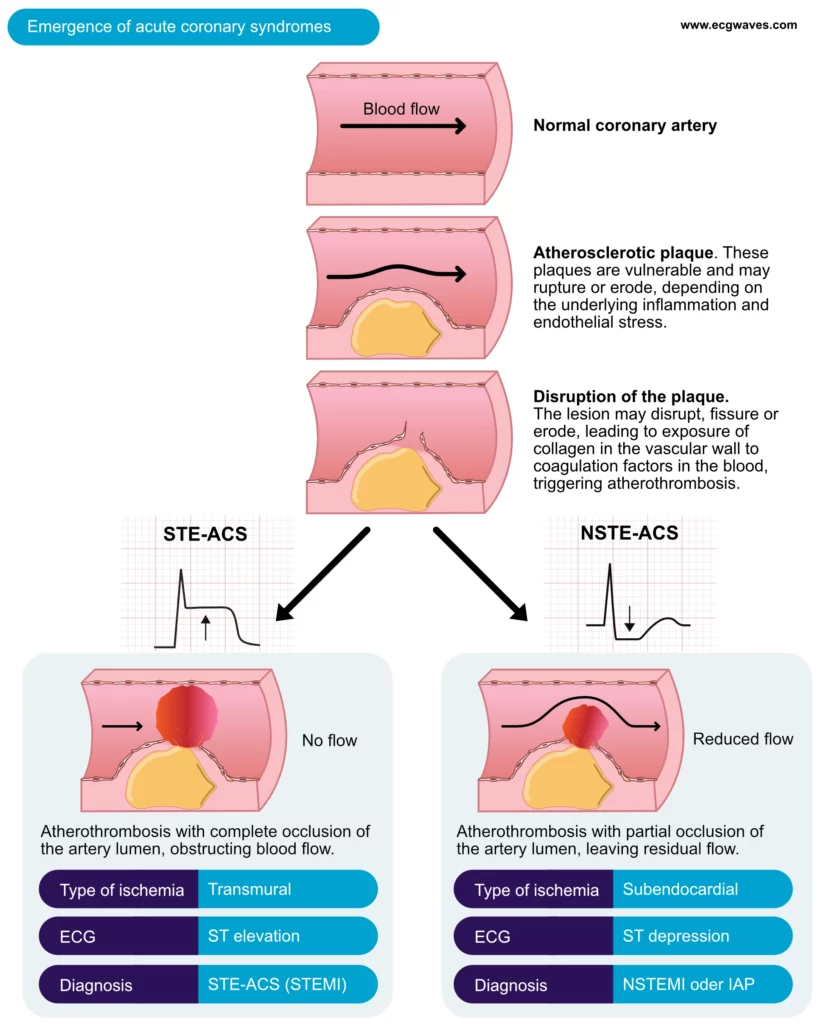
Acute coronary syndromes occur when atherosclerotic plaques disrupt, resulting in the activation of thrombocytes and coagulation factors causing the formation of a thrombus. Such a thrombus can cause occlusion of the artery. The occlusion may be complete or partial, depending on the size of the thrombus and the plaque. The patient will experience severe chest pain due to the abrupt reduction of coronary blood flow. Acute coronary syndromes are subdivided into STE-ACS and NSTE-ACS. STE-ACS is the acronym for ST Elevation Acute Coronary Syndrome. All acute coronary syndromes that exhibit significant ST segment elevations on ECG are classified as STE-ACS. Moreover, STE-ACS is caused by a complete coronary artery occlusion and virtually all these patients will develop myocardial infarction, which is classified as STEMI (ST Elevation Myocardial Infarction).
NSTE-ACS is the acronym for Non-ST Elevation Acute Coronary Syndrome. This category includes all acute coronary syndromes without significant ST segment elevations on ECG. NSTE-ACS is caused by partial occlusion of the artery (i.e. coronary blood flow is not completely obstructed). NSTE-ACS typically presents with ST segment depressions and/or T-wave inversions. Most patients with NSTE-ACS will develop acute myocardial infarction, which is then classified as NSTEMI (Non-ST Elevation Myocardial Infarction). Patients with NSTE-ACS who do not develop infarction are classified as unstable angina (UA), which is an imminent precursor to myocardial infarction. NSTEMI and unstable angina have similar pathophysiology and management are also similar. Hence, the difference between STE-ACS and NSTE-ACS is merely the presence of ST segment elevations in the former.
Refer to Figure 1, which illustrates the natural course of coronary artery disease, from risk factors to acute coronary syndromes. It also presents a classification of acute coronary syndromes and myocardial infarctions. The reader should study this chart carefully.
Acute myocardial infarction: a diagnosis based on cardiac troponins
A diagnosis of acute myocardial infarction (AMI) is made only after blood analyses confirm elevated levels of myocardial proteins. These proteins are cardiac troponins (henceforth referred to only as troponins). When elevated troponin levels are confirmed in patients with STE-ACS, the condition is classified as STEMI (ST elevation myocardial infarction). When elevated troponin levels are confirmed in patients with NSTE-ACS, the condition is classified as NSTEMI (Non-ST elevation myocardial infarction). If troponin levels are normal in patients with NSTE-ACS, the condition is classified as unstable angina (UA). Please refer to Diagnostic Criteria for Myocardial Infarction for further details.
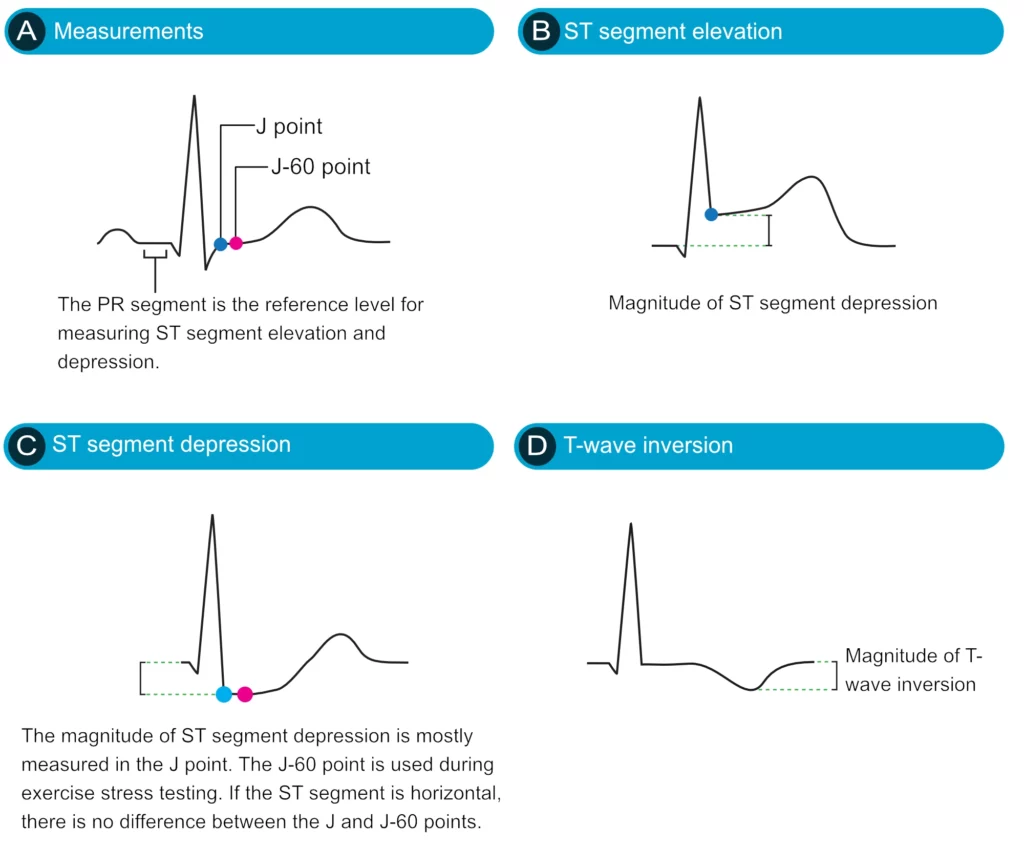
Figure 2 (below) displays ST segment depression, ST segment elevation and T-wave inversion. These ECg changes will be discussed in great detail in the subsequent chapters.
STE-ACS (ST Elevation Acute Coronary Syndrome) & STEMI (ST Elevation Myocardial Infarction)
Acute coronary syndromes with significant ST segment elevations are classified as STE-ACS. Virtually all cases of STE-ACS lead to myocardial infarction (elevated troponin levels), whereafter the condition is classified as ST Elevation Myocardial Infarction (STEMI). The thrombus causing STE-ACS is located proximally in the coronary artery and it occludes the entire artery lumen (i.e. no blood passes the thrombus). The ensuing ischemia is transmural, implying that it is extensive and stretches from the endocardium to the epicardium (Figures 1 and 2).
ECG characteristics of STE-ACS (STEMI)
The ECG leads which display ST segment elevations reflect the ischemic area. This means, for example, that ST segment elevations in leads V3 and V4 (anterior chest leads) reflect transmural anterior ischemia. ST elevations must exist in at least two anatomically contiguous leads in order to fulfill the criteria for STE-ACS. Anatomically contiguous implies that the leads must be anatomically juxtaposed; for example V1 and V2; V5 and V6; V4 and V5; aVF and III and so on. In most cases, the ST segment elevations are accompanied by reciprocal ST segment depressions. Such ST segment depressions occur in leads that detect the ischemic vectors from the opposite angle, compared with the leads showing ST segment elevations. The ST segment elevations are gradually normalized and followed by T-wave inversions. The latter may persist for a month, or even longer.
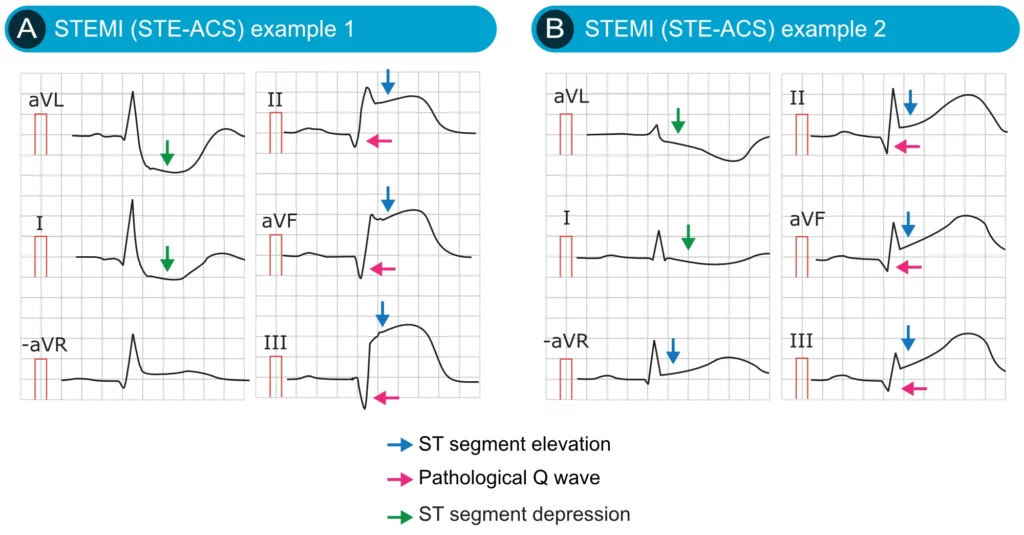
Pathological Q-waves may appear if the infarct area is large. These Q-waves are abnormally wide and deep. They testify that the heart has suffered a large infarction. Infarctions that leave pathological Q-waves are referred to as Q-wave infarctions.
On very rare occasions the thrombus may resolve (either spontaneously or due to fast reperfusion treatment) before the infarction process begins. In this case, the troponin levels are not elevated and the condition is classified as unstable angina (or aborted myocardial infarction). This is, however, rare because virtually all cases of STE-ACS progress to STEMI.
Patients with STE-ACS (STEMI) have pronounced symptoms (notably chest pain) and a high risk of ventricular arrhythmias in the acute phase. This is because the ischemic area is extensive. Potentially life-threatening ventricular arrhythmias (ventricular tachycardia and ventricular fibrillation) may occur and such arrhythmias cause virtually all deaths in the acute phase of STEMI (and in acute coronary syndromes in general). Death due to pumping failure (cardiogenic shock) is much less common in the acute phase.
NSTE-ACS (Non ST Elevation Acute Coronary Syndrome): NSTEMI (Non-ST Elevation Myocardial Infarction) & Unstable Angina
All acute coronary syndromes which do not fulfill the criteria for STE-ACS are automatically classified as NSTE-ACS. The artery occlusion is partial (not complete) and thus some blood flow remains in the artery. The occlusion is typically located proximally (along the epicardial course of the artery).
Because the occlusion is partial the ischemia will primarily affect the subendocardium, which has the poorest prerequisites in the case of ischemia. This is explained by the following:
- The subendocardium is too far away from the blood in the ventricular cavity. Hence, oxygen within the ventricle does not reach the subendocardium (it does, however, reach the endocardium).
- The oxygen level in the coronary artery reaching the subendocardium is reduced because oxygen is extracted during the passage through the epicardial layers.
These two factors explain why the subendocardium has poor prerequisites in the setting of acute coronary syndromes.
NSTE-ACS is classified as Non-ST Elevation Myocardial Infarction (Non-STEMI, NSTEMI) if troponin levels are elevated. If cardiac troponin levels are normal, the condition is classified as unstable angina pectoris, which thus can be viewed as an impending myocardial infarction (Figures 1 & 2).
ECG characteristics of NSTE-ACS (NSTEMI, unstable angina)
The hallmark of NSTE-ACS (NSTEMI) is ST segment depressions which are often accompanied by T-wave changes. The latter may be T-wave inversions or flat T-waves. Importantly, the leads displaying ST segment depressions do not necessarily reflect the ischemic area. This means that ST segment depressions in leads V3–V4 are not necessarily due to anterior wall ischemia. Similarly, ST segment depressions in leads II, aVF and III do not suggest inferior wall ischemia. Hence, ST-segment depressions cannot localize the ischemic area. Please refer to Localization of Acute Myocardial Infarction and Culprit Artery for details on how to localize the ischemia/infarction using ECG.
Pathological Q-waves usually do not develop, which is explained by the fact that NSTEMI is generally smaller infarctions than STEMI. However, extensive subendocardial infarctions may certainly lead to pathological Q-waves. It is actually a widespread misunderstanding that infarctions must be transmural in order to cause pathological Q-waves.
T-wave inversions are also frequently misunderstood. Isolated T-wave inversions, i.e. T-wave inversions without concomitant ST segment deviations, are never indicative of acute (ongoing) ischemia. T-wave inversions that are accompanied by ST segment depressions, however, are indicative of acute (ongoing ischemia), but in that scenario, it is actually the ST segment deviation that reflects the ischemia. Isolated T-wave inversions are post-ischemic, i.e. they occur after the ischemic episode has surmounted.
A minority of patients with NSTE-ACS (Non-STEMI) display normal ECG on arrival. It is unusual, however, to display a normal ECG throughout the course; the majority of patients with normal ECG on arrival will develop some ECG changes during the course. Moreover, normal ECGs on arrival cannot be used to rule out myocardial ischemia/infarction. There are infarctions that do not cause ECG changes (typically smaller infarctions) and there are cases in which the thrombus is dynamic in size. The thrombus may become larger or smaller, with minute-to-minute variation, and thus cause varying ECG changes.
NSTE-ACS (Non-STEMI) is treated with anti-ischemic, anti-thrombotic medications. Most patients undergo coronary angiography with the purpose of performing PCI. Angiography is performed within 24 hours but sooner if the patient is a high-risk patient. ECG changes, troponin levels, clinical status and comorbidities will dictate if angiography must be performed promptly. Note that immediate angiography (as is done in STE-ACS/STEMI) has not reduced mortality or morbidity in NSTE-ACS (Non-STEMI), which is why guidelines recommend subacute angiography.
Last but not least, NSTE-ACS may actually occur due to a proximal and complete occlusion (which usually leads to STE-ACS) if the affected myocardium has extensive collateral circulation. Collateral circulation, which is common among patients with coronary artery disease, implies that the ischemic area obtains blood flow from two coronary arteries (or branches of arteries). This type of circulation arises when ischemic myocardium stimulates surrounding arteries to sprout out vessels to the ischemic area (VEGF [Vascular Endothelial Growth Factor] plays a critical role in the development of collateral circulation).
Figure 6 (below) summarizes the classification of acute myocardial infarction and coronary syndromes.
Normalization of ECG changes
ST-T changes are normalized within days or weeks. The duration is longer if ischemia results in infarction. QRS changes are mostly permanent, particularly Q-waves. Note that treatment and reperfusion therapy may modify the speed by which the ECG normalizes.
Risk stratification in patients presenting with acute coronary syndromes: TIMI and GRACE score
Early risk assessment can improve outcomes in patients with acute coronary syndromes. Such risk assessment should address the probability that the syndrome is an acute coronary syndrome and, secondly, the probability of adverse outcomes (myocardial infarction and death). Several validated models (“risk calculators”) have been developed to simplify risk stratification. These models typically include information regarding medical history, ECG findings, presenting features (notably hemodynamic status), and cardiac troponins. The best-validated risk models are FRISC II, TIMI, PURSUIT, and GRACE. These vary concerning the type of risk estimated (short-term, long-term, myocardial infarction, death). TIMI score is the easiest to use but the GRACE score has proven to be the most accurate. Moreover, GRACE is applicable to both NSTEMI and STEMI.

