Sinus tachycardia: causes, ECG, normal variants & pathological variants
Sinus tachycardia is the most common tachyarrhythmia (tachycardia). Sinus tachycardia is the result of an increased rate of depolarization (i.e increased automaticity) in the sinoatrial node. This simply means that the sinoatrial node discharges electrical impulses at a higher frequency than normal. Similar to sinus rhythm, the rhythm is regular with a positive P-wave in lead II, but the heart rate exceeds 100 beats per minute.
Although sinus tachycardia is the most common tachyarrhythmia, it may not always be straightforward to diagnose on the ECG. Moreover, many clinicians remain uncertain about the implications of sinus tachycardia. A crucial task is to distinguish three types of sinus tachycardia. These types differ fundamentally in terms of pathophysiology, prognosis, and treatment. The types of sinus tachycardia are as follows:
- Normal (physiologic) sinus tachycardia: The automaticity (rate of spontaneous depolarization) in the sinoatrial node is increased during physical activity, stress, and nervousness. This is due to altered tone in the autonomic nervous system, with increased sympathetic input (leading to stimulation of beta-adrenergic receptors) and parasympathetic withdrawal.
- Sinus tachycardia secondary to disease and medications: A wide range of diseases and medications may cause sinus tachycardia; e.g congestive heart failure, lung disease (e.g COPD), fever, infections, anemia, myocardial ischemia/infarction, pulmonary embolism, pheochromocytoma, hyperthyroidism, hypovolemia, pharmacological substances (alcohol, amphetamine, coffee, anticholinergic drugs, beta-adrenergic agonists). In all of these conditions, sinus tachycardia is merely an expression of an underlying disease or substance effect, which may require attention. Therefore, management of sinus tachycardia always requires that each of these causes be assessed thoroughly, as many of the causes require prompt treatment.
- Inappropriate sinus tachycardia: When all the abovementioned causes have been ruled out and the sinus tachycardia persists without any known cause, it may be classified as inappropriate sinus tachycardia. This diagnosis can only be established after all other causes have been ruled out. Inappropriate sinus tachycardia is presumably more common than previously thought and the condition may hamper the quality of life substantially.
The management of sinus tachycardia is aimed at finding secondary causes that can be treated or, when no cause can be found, establishing a diagnosis of inappropriate sinus tachycardia. Although there are no evidence-based treatments for inappropriate sinus tachycardia, patients frequently benefit from obtaining a diagnosis, because it justifies their symptoms (treatment alternatives are discussed below).
ECG in sinus tachycardia
Sinus tachycardia fulfills all criteria for sinus rhythm but the heart rate is faster than 100 beats per minute. Thus, the ECG criteria for sinus tachycardia follow.
ECG criteria for sinus tachycardia
- Regular rhythm with ventricular rate >100 beats per minute.
- P-wave with constant morphology preceding every QRS complex.
- The P-wave is positive in lead II.
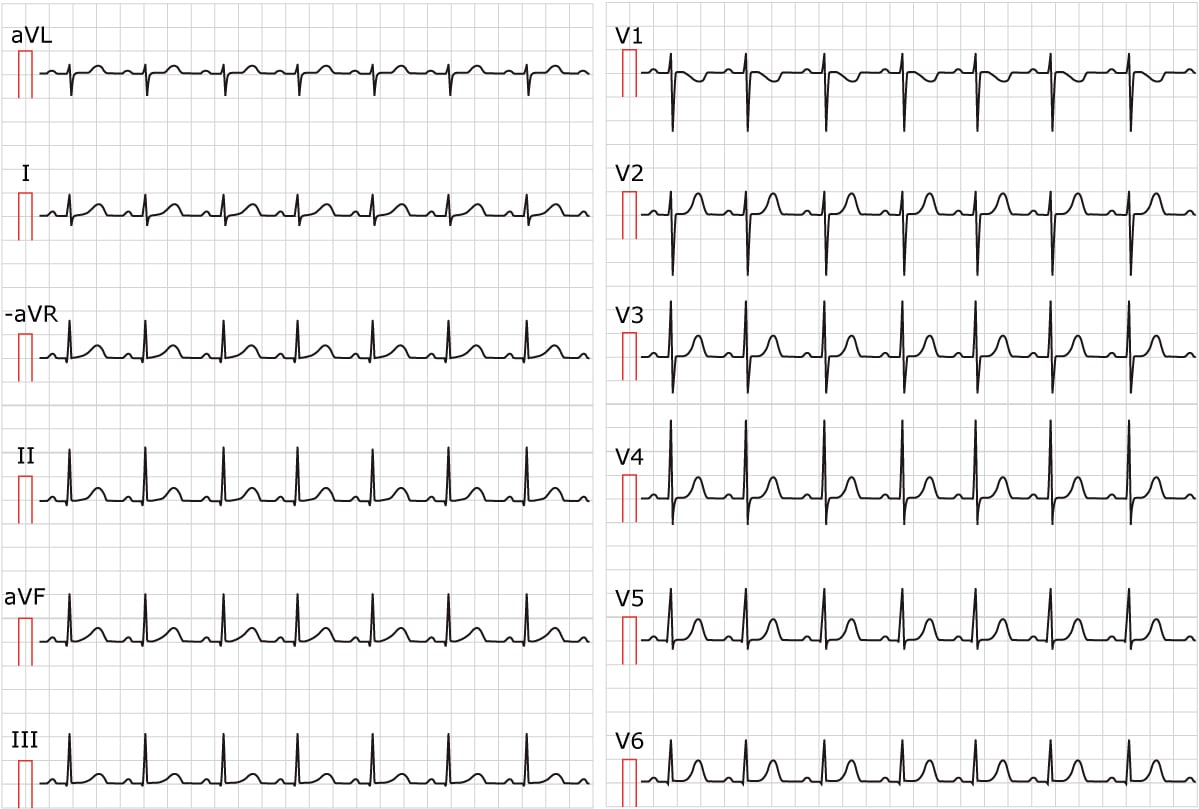
ECG characteristics of sinus tachycardia
Note that at heart rates above 140 beats per minute, it may be difficult to discern the P-waves from the previous T-wave, particularly if the paper speed is 25 mm/s (using 50 mm/s may be advised). Always search carefully for the P-wave as it may be very discrete and only cause an irregularity of the contour of the T-wave. Finding the P-wave is a requirement for establishing a diagnosis of sinus tachycardia.
On the contrary to many paroxysmal supraventricular tachyarrhythmias (e.g AVNRT, AVRT, or atrial tachycardia), sinus tachycardia has a gradual onset and the patient can often report that the palpitations accelerated gradually. Note that the mode of onset (abrupt vs. gradual) is an important piece in the puzzle to determine which type of arrhythmia a patient suffers from. Abrupt onset suggests that the tachyarrhythmia is AVNRT, AVRT, atrial tachycardia, atrial flutter or atrial fibrillation. It may, however, also be a special form of sinus tachycardia referred to as SANRT (discussed below).
Long-standing sinus tachycardia may lead to ST-segment depressions on the ECG. Such ST-segment depressions may be seen anywhere but most commonly in leads V3, V4, V5 and V6. The ST-segment tends to be either horizontal or upsloping. Long-standing sinus tachycardia may also cause diminished T-wave amplitude on the ECG. This occurs in the same leads that display ST-segment depressions. These ST-segment depressions and diminished T-wave amplitude should disappear rapidly (within minutes) after the sinus tachycardia has resolved. Otherwise, one must suspect other causes of ST-segment depression (e.g. acute myocardial ischemia).
Sinus tachycardia with strong sympathetic activation has a bathmotropic effect on the conduction system. This implies that the speed of impulse conduction is increased. Therefore, the PR interval may be slightly (but not significantly) reduced. Long-standing and rapid sinus tachycardia, on the other hand, may exhaust the atrioventricular node and bring about a slowing of conduction that prolongs the PR interval (again, not significantly).
Maximum heart rate
It is often difficult to differentiate sinus tachycardia from other supraventricular tachycardias (e.g. atrial flutter, AVNRT etc). Many of these tachycardias have a tendency to present themselves with a particular heart rate. There is an age-dependent upper limit for the impulse frequency of the sinoatrial node. The maximal discharge rate in the sinoatrial node diminishes with age (due to diminishing sensitivity to catecholamines). Hence, using the individual expected maximum sinus rate may help differentiate sinus tachycardia from other arrhythmias. Any tachycardia with a rate faster than the age-expected maximum rate is probably not sinus tachycardia.
The maximum discharge rate in the sinoatrial node is estimated using the following formulas:

Note that at maximal exercise capacity, the sinus rate may be somewhat higher than the formula estimate. Also note the third formula, which is necessary to estimate a maximum frequency in patients using beta-blockers (which diminish the discharge frequency of the sinoatrial node).
Normal range for sinus rhythm
The lower limit of sinus tachycardia is 100 beats per minute and this is an arbitrary and questioned figure. The main reason for this is that observational studies (both retrospective and prospective) and randomized controlled clinical trials have shown that the association between heart rate and mortality is linear, and mortality increases gradually at heart rates above 60 beats per minute. Moreover, studies in recent years show that resting heart rate is a strong predictor of overall and cardiovascular mortality.
Inappropriate sinus tachycardia
Inappropriate sinus tachycardia is a condition where sinus tachycardia is present at rest and the sinus rate is usually excessively high during physical activity. The condition has been recognized for more than seven decades but many clinicians are still unaware of it. A large body of science suggests that inappropriate sinus tachycardia is caused by increased automaticity in the sinoatrial node. The cause of the increased automaticity, however, remains elusive. Theories suggest hypersensitivity to catecholamines, disturbance in the autonomic nervous system, etc. Inappropriate sinus tachycardia may only be diagnosed when all other causes of sinus tachycardia have been ruled out.
Patients with sinus tachycardia present with a resting heart rate above 100 beats per minute. They also tend to have an excessive increase in heart rate during all sorts of physical activity. Their heart rate during sleep is higher than the average individual. For some unexplained reason women, particularly health care workers, are overrepresented. Pre-syncope, syncope, chest discomfort, dyspnea, anxiety and fatigue are also common symptoms.
No clear evidence points to any increased mortality in inappropriate sinus tachycardia. This is somewhat unexpected given that tachycardia is a well-known risk factor for cardiomyopathy (tachycardia-induced cardiomyopathy). It is not unlikely that individuals with inappropriate sinus tachycardia will be at greater risk of cardiovascular disease but the evidence is yet lacking.
Management of high resting heart rate and inappropriate sinus tachycardia (IST)
Non-pharmacological Interventions
First-line management includes lifestyle modifications:
- Avoidance of stimulants (e.g., caffeine, nicotine, alcohol).
- Regular aerobic exercise to improve autonomic balance.
- Adequate hydration and increased salt intake to support plasma volume.
- Use of compression garments and elevating the head of the bed to mitigate orthostatic symptoms .
Pharmacological therapy
- Beta-blockers: Agents like bisoprolol (5–10 mg once daily) are commonly used but may have limited efficacy and tolerability due to side effects such as fatigue and hypotension.
- Ivabradine: A selective If current inhibitor that reduces heart rate without affecting blood pressure or myocardial contractility. Studies have shown its effectiveness in IST patients, particularly those intolerant to beta-blockers.
- Calcium channel blockers: Non-dihydropyridine agents (e.g., verapamil) may be considered, though evidence for their efficacy in IST is limited.
Interventional approaches
Catheter ablation targeting the sinus node has been attempted in refractory cases. However, this approach carries significant risks, including the potential need for permanent pacemaker implantation, and is generally reserved for patients with debilitating symptoms unresponsive to medical therapy.
Sinoatrial nodal re-entrant tachycardia (SANRT)
Sinoatrial nodal re-entrant tachycardia (SANRT) is caused by a re-entry circuit in or by the sinoatrial node. It is recognized on the ECG (typically requires ECG monitoring for a longer period) as abruptly starting sinus tachycardia. Normal sinus tachycardia does not start abruptly, but rather gradually. The P-wave in SANRT is identical to the sinus P-wave. Other terms used for this condition are sinus node reentry or sinus node reentrant tachycardia.
