Management and treatment of AV block (atrioventricular blocks)
Management and treatment of AV blocks (AV-block 1, 2 & 3)
Evaluation of patients with suspected AV blocks requires a thorough medical history (with emphasis on causes of AV blocks; please refer to the Causes of AV blocks) and physical examination. It is also reasonable to analyze cardiac troponins if there is any probability of myocardial ischemia as the underlying cause. Holter ECG may be valuable if the diagnosis is uncertain. Echocardiography is generally performed in order to evaluate ventricular function, since it may affect the choice of device therapy and also suggest whether other interventions (e.g. heart failure management, evaluation for coronary artery disease, etc.) are warranted. Management of AV blocks aims to restore atrioventricular conduction either pharmacologically or by means of artificial pacemakers. Both methods may be used in the acute setting, whereas long-term management only includes pacemaker therapy.
Treatment of AV block in the acute setting
Treatment in the acute setting is directed at managing bradycardia and reduced cardiac output. Bradycardia causing hemodynamic instability is a potentially life-threatening condition and should be managed urgently. The risk of cardiogenic shock is high and pharmacological interventions are often futile. A transcutaneous pacemaker is often necessary in the acute setting and is currently the only treatment with class I recommendation according to European (ESC) and North American (AHA, ACC) guidelines. For details regarding the management of bradycardia, please refer to Management of acute bradycardia. A summary of the treatments is provided below.
In the event of manifest or impending circulatory collapse, transcutaneous pacing must be started immediately. The risk of circulatory collapse is highest with AV block 2 Mobitz type 2 and AV block 3. The only treatment with a class I recommendation for the management of acute bradycardia is transcutaneous pacing. Pharmacological interventions (Table 4) should be considered temporary, often insufficient, treatments that can be attempted until a pacemaker is established.
| Drug | Effect | Dose, kinetics | Comment |
|---|---|---|---|
| Atropine | Acetylcholine receptor antagonist | 1 mg IV every 3-5 minutes, maximum 3 mg IV. T½ 3 h. 50% renal elimination. | • Typically the first choice of drug. • Effective in sinus bradycardia or AV node block. • Dose <0.5 mg may worsen bradycardia and should not be given. • Relative contraindications are ileus, glaucoma. |
| Isoprenaline / Isoproterenol | α-1, α-2, β-1, β-2 agonist | Start infusion at 4 μg/min and titrate to desired result T½ 1 min | • May cause ventricular arrhythmias (dose-dependent). • Prolonged use often causes headaches, tremors. • Effective if bradycardia is caused by beta blockers. |
| Adrenaline (Epinephrine) | α and β agonist | Infusion of 2–10 μg/min (titrate as needed). T½ 5 min. | • Effective if hypotension is present. • Can be given as a bolus. • Effective if bradycardia is caused by beta blockers. |
| Dopamine | Dopamine receptor agonist, α- and β-agonist | Infusion of 5−20 μg/kg/min T½ 2 min | • Avoid boluses. • Effective if bradycardia is caused by beta blockers. |
| Dobutamine | β-1 agonist | Infusion of 3−10 μg/kg/min. T½ 2 min | Effective if inotropic effect is required. |
| Theophylline / theophyllamine / aminophylline | Adenosine receptor antagonist, phosphodiesterase inhibitor. Exact mechanism is unknown. | 100−200 mg slow iv injection. | Rarely used. |
| Glucagon | Counteracts beta blockers. An antidote to beta blockers. | 2–10 mg bolus followed by 2–5 mg/h infusion | Antidote to beta blockers. |
| Calcium | Counteracts calcium channel blockers (CCB). Antidote to CCBs. | 10 ml calcium 0.2 mmol/ml iv. | Antidote to CCBs. |
| Digoxin antibodies | Binds to digoxin. | Digitalis antidote (anti-digoxin, Fab fragment). | Given in case of suspected digoxin intoxication. |
Atropine
Evidence: Class IIa recommendation
- Atropine is the first choice for the pharmacological treatment of acute bradycardia.
- Dosage: 1 mg iv, every 3-5 minutes, to a maximum of 3 mg.
- Doses lower than 0.5 mg IV may worsen bradycardia and should never be given.
- The effect of atropine is temporary.
- If atropine is ineffective, isoprenaline, adrenaline (epinephrine) or dopamine can be tried.
- Atropine counteracts acetylcholine-mediated bradycardia by inhibiting the effect of acetylcholine on the sinus node and AV node. Atropine is effective in sinus bradycardia and AV block located in the AV node.
- Atropine is typically ineffective in complete AV block and Mobitz type 2 second-degree AV block.
- Atropine is not used in patients with heart transplantation.
Isoprenaline (isoproterenol)
Evidence: Class IIa recommendation
- Isoprenaline is a second-line pharmacological treatment for acute bradycardia.
- Dosage: Start infusion at 4 μg/min and titrate to the desired result.
- Half-life: 5 minutes.
- Isoprenaline enhances AV conduction in nodal blocks. In infranodal blocks, isoprenaline is effective only if it induces an escape rhythm, or enhances the automaticity of an existing escape rhythm.
Adrenaline (epinephrine)
Evidence: Class IIb recommendation
- Effective in hypotension and when an inotropic effect is required.
- Dosage: Infusion of 2–10 μg/min (titrate as needed).
- Can be added to dopamine.
Dopamine
Evidence: Class IIb recommendation
- Effective in hypotension and when an inotropic effect is required.
- Dosage: Infusion 5−20 μg/kg/min.
- Can be added to adrenaline.
Temporary pacemaker
Transcutaneous pacemaker
Evidence: Class I recommendation
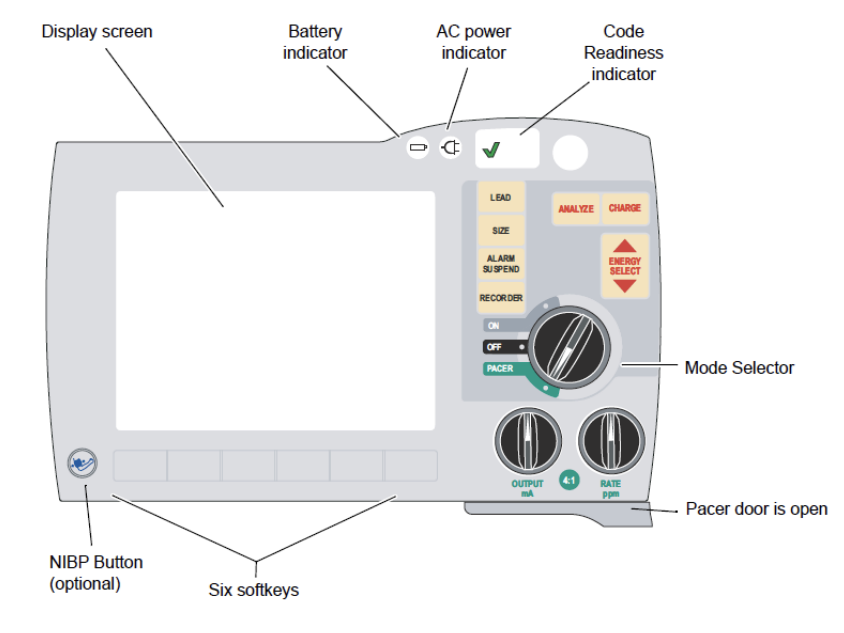
Most defibrillators have a pacemaker function, allowing the device to operate as an external pacemaker. (Video 1, Figure 2, Figure 3).
- A pacemaker is the safest treatment for acute bradycardia.
- A transcutaneous pacemaker should be established immediately if there is a risk of hemodynamic collapse.
- AV block 2 Mobitz type 2 and AV block 3 are strong indications for a transcutaneous pacemaker.
Pain and discomfort during transcutaneous pacing
Although transcutaneous pacing can be unpleasant or somewhat painful, all patients tolerate the procedure. Pain is caused by muscle contractions. Administration of sedatives (midazolam) or analgesics (morphine) is recommended, using the following doses:
- Midazolam: 1–3 mg initial dose. Total dose 4-8 mg. Lower dose range in cases aged >60 years.
- Morphine: 2.5 mg IV.
How to perform transcutaneous pacing
- Explain to the patient the purpose of the procedure.
- Administer sedatives / analgesics.
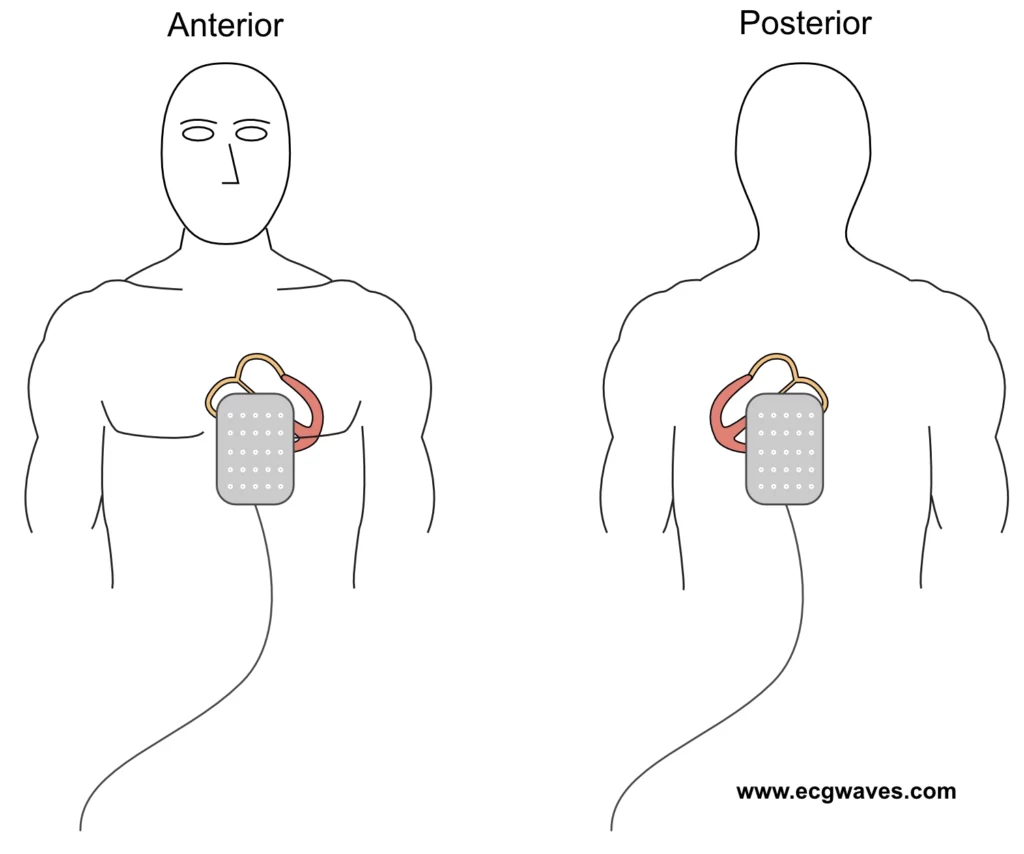
- Position electrode pads in anteroposterior direction (Figure 4).
- If there is time, trim chest/back hair (do not shave). Dry the skin if wet.
- Do not relocate already attached pads (the adhesive becomes poor).
- Activate the pacemaker function (Video 1, Figure 2, Figure 3).
- Set the pacing rate to 50 beats/min.
- Gradually increase the current (start with 20 mA).
- Identify the pacemaker spikes (stimulation artifacts) on the ECG recording.
- Determine if pacemaker spikes are followed by QRS complexes (indicating electrical capture).
- If electrical capture is visible, palpate the femoral artery to examine whether there is mechanical capture (i.e. ventricular contractions).
- Monitor blood pressure and pulse oximetry.
- When the threshold for capture (lowest current producing mechanical capture) is identified, the output (current) is increased by 10% (in order to provide stimulations with a safety margin).
- Most patients require a current in the range of 20 to 140 mA
- Avoid unnecessary pacing by using a low base frequency (e.g. 30–40 beats/min).
How to perform transcutaneous pacing during asystole
Follow the same procedure as above but start with maximum current strength (output) and gradually reduce the current until stimulation fails to produce capture. Then increase the current until capture is obtained, and another 10% output as a safety margin.
Checking transcutaneous pacing
- Mechanical capture is confirmed by palpating a peripheral pulse (femoral artery) or assessing pulse oximetry. Avoid evaluating the pulse in the carotid artery (pectoral muscle contractions may be mistaken as arterial pulsations).
- Muscle contractions are not equivalent to mechanical capture.
- If the pacemaker stimulates more than necessary, there is undersensing, which means that the pacemaker does not detect the ventricular complexes (and therefore continues to pace). This is resolved by relocating the ECG leads so that they detect larger QRS amplitudes or increasing the gain on the defibrillator.
- If the pacemaker does not stimulate due to artifacts there is oversensing, which can be resolved by eliminating the artifacts or relocating the leads.
Transvenous pacing
- A transvenous pacemaker should be established if transcutaneous pacing is ineffective.
- Transvenous pacemaker requires higher competence to establish and also entails a risk of infection, perforation and tamponade.
- Access can be obtained via the jugular vein or the femoral vein. The introduction of a pacemaker lead via the jugular vein carries a risk of local thrombosis or infection, which complicates later pacemaker implantation. Pacing via the femoral vein requires immobilization of the patient since movements can cause dislocation of the lead.
- A transvenous pacemaker can use a screw electrode, which can remain for up to 6 weeks and carries a significantly lower risk of lead dislocation.
Long-term treatment
- First-degree AV block and second-degree AV block Mobitz type I: These AV blocks rarely require therapy, unless the patient is symptomatic. A pacemaker is indicated in patients who are clearly symptomatic, particularly if they display a wide QRS complex.
- Second-degree AV block Mobitz type II and third-degree AV block: These cases should almost invariably receive a pacemaker. In the case of Mobitz type 2 with wide QRS complexes, a pacemaker is indicated even in the absence of symptoms. All cases of third-degree AV block necessitate a pacemaker.
Related articles
