Sinus bradycardia: definitions, ECG, causes and management
Sinus bradycardia: ECG, causes & management
Definition of sinus bradycardia
Sinus bradycardia fulfills the criteria for sinus rhythm but the heart rate is slower than 50 beats per minute. ECG criteria follows:
- Regular rhythm with ventricular rate slower than 50 beats per minute.
- P-waves with constant morphology preceding every QRS complex.
- P-wave is positiv in limb lead II.
Normal (physiological) causes of sinus bradycardia
Sinus bradycardia (SB) is considered a normal finding in the following circumstances:
- During sleep.
- Well-trained individuals display SB at rest due to high vagal tone. These individuals have developed a highly efficient left ventricle, capable of generating sufficient cardiac output at low heart rates.
- During vasovagal syncope (e.g during intense emotional stress)
- During vagal maneuvers (Valsalva maneuver, carotid sinus [baroreceptor] stimulation).
- Its not uncommon to discover SB in healthy young individuals who are not well-trained. This is also a normal finding.
Abnormal (pathological) causes of sinus bradycardia
In all other situations, sinus bradycardia should be regarded as a pathological finding. There are numerous pathological conditions that cause sinus bradycardia. The most important causes are as follows:
- Myocardial ischemia/infarction – Particularly ischemia or infarction located to the inferior wall of the left ventricle. This type of bradycardia is due to diminished automaticity (pacemaker function) in the sinoatrial node or conduction defects (e.g second-degree AV block) as a result of ischemia/infarction.
- Sinus Node Dysfunction (SND) – Sinus node dysfunction implies that the cells of the sinoatrial node are defect and fail to generate electrical impulses.
- Side effects of drugs (notably beta blockers, digitalis, verapamil, diltiazem, amiodarone, klonidin) – These drugs affect the pacemaker cells in the sinoatrial node. They may also induce conduction defects (e.g AV block).
- Increased intracranial pressure (manifests with sinus bradycardia and hypertension).
- Hypothyroidism.
- Hypothermia.
- Hyperkalemia.
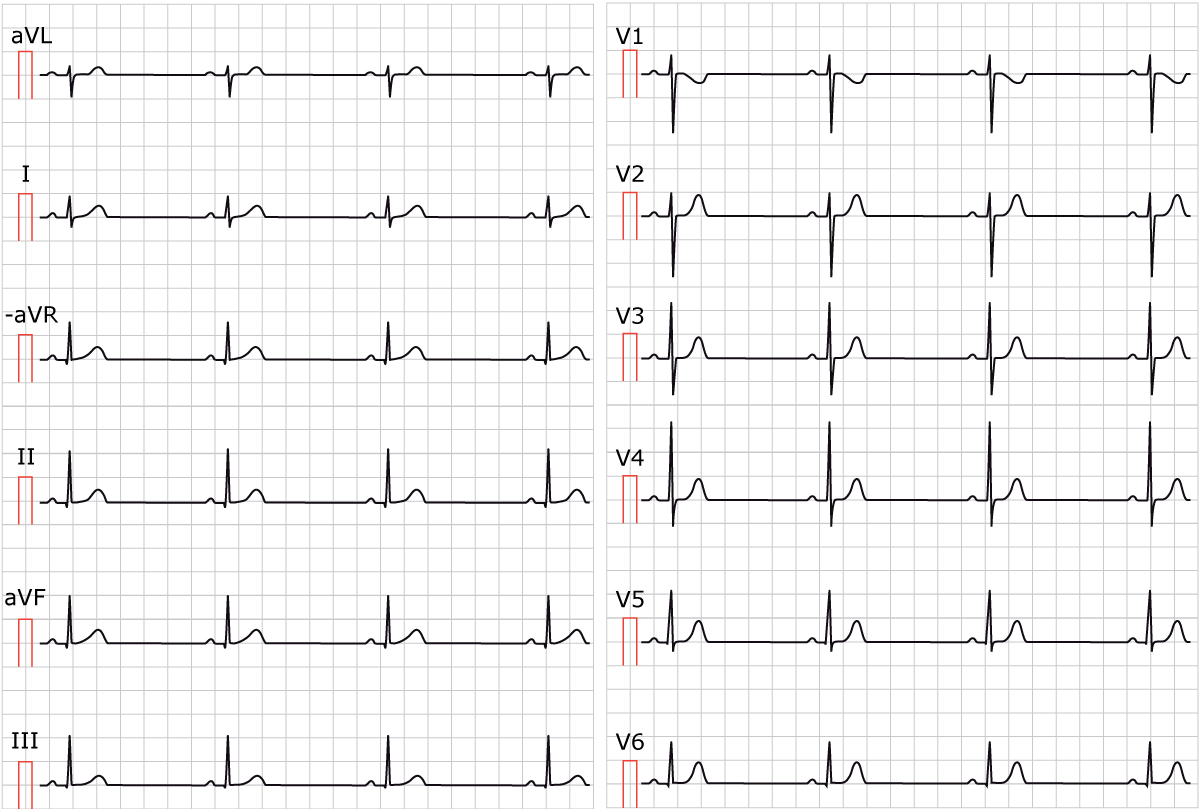
ECG example of sinus bradycardia
Figure 1 shows sinus bradycardia at paper speed 25 mm/s.

Treatment of sinus bradycardia
Benign causes of sinus bradycardia (e.g. vasovagal reaction, well-trained athletes) do not require treatment. When benign causes are unlikely, it is necessary to identify reversible causes, in order to direct targeted interventions toward them. A permanent pacemaker is generally indicated when reversible causes are absent and the patient is symptomatic or at risk of developing symptoms.
The most common non-reversible causes of sinus bradycardia are sinus node dysfunction, side effects of medications and acute myocardial infarction.
Holter ECG is useful to determine the frequency, severity and situational dependence of sinus bradycardia. If sinus bradycardia is likely due to drug side effects, it is necessary to weigh the risk of terminating the medication as compared with implanting a permanent pacemaker and continuing the treatment. It is common that patients with bradycardia have a strong indication for drugs that aggravate or cause bradycardia (e.g. beta-blockers in heart failure). In such scenarios, it is very common to provide the patient with a permanent pacemaker in order to continue optimal medical treatment.
Sick sinus syndrome (sinus node dysfunction), which is a common cause of bradycardia, is also discussed separately.
Algorithm for acute management of bradycardia
Treatment of acute bradycardia is discussed in the following chapter:
Please refer to the chapter referenced above for details. In summary, acute bradycardia is managed as follows:
- Terminate or adjust any medications that cause or aggravate the bradycardia.
- If bradycardia causes hemodynamic effects (reduced cardiac output or hypotension), the following algorithm is used:
- Prepare an external pacing device (e.g. a defibrillator with pacing function and position the electrodes in anterior-posterior position. Prepare to administer a sedative (e.g. midazolam) or analgesic (e.g. morphine) during transcutaneous pacing.
- Immediately give 1 mg atropine iv. Repeat up to 3 mg.
- If atropine is insufficient, start infusion of isoproterenol. An ampoule with 5 ml (0,2 mg/ml) isoproterenol is mixed with 245 ml glucose (50 mg/ml) with starting dose 0,01 μg/kg/min. This is titrated up until adequate effect is achieved.
- Transcutaneous pacing (external pacing) is started if atropine and isoproterenol fail. Transcutaneous pacing is indicated until a temporary transvenous pacemaker can be implanted.
Patients with bradycardia due to myocardial ischemia or infarction only require treatment if cardiac output is reduced or if the bradycardia predisposes to malign ventricular arrhythmias (the algorithm above applies to this situation as well). However, bradycardia due to inferior wall ischemia or infarction is mostly transient and rarely necessitates a permanent pacemaker. Bradycardia due to anterior wall infarction, however, is mostly permanent and requires a pacemaker.
Permanent (long-term) treatment of bradycardia
Permanent symptomatic bradycardias are treated with pacemakers.
 Next chapter
Next chapter
 Related chapters
Related chapters
Normal automaticity and pacemaker cells in the heart
Mechanisms of cardiac arrhythmias
Sinus tachycardia & Inappropriate Sinus Tachycardia

