Right bundle branch block (RBBB): ECG, criteria, definitions, causes & treatment
Right bundle branch block (RBBB)
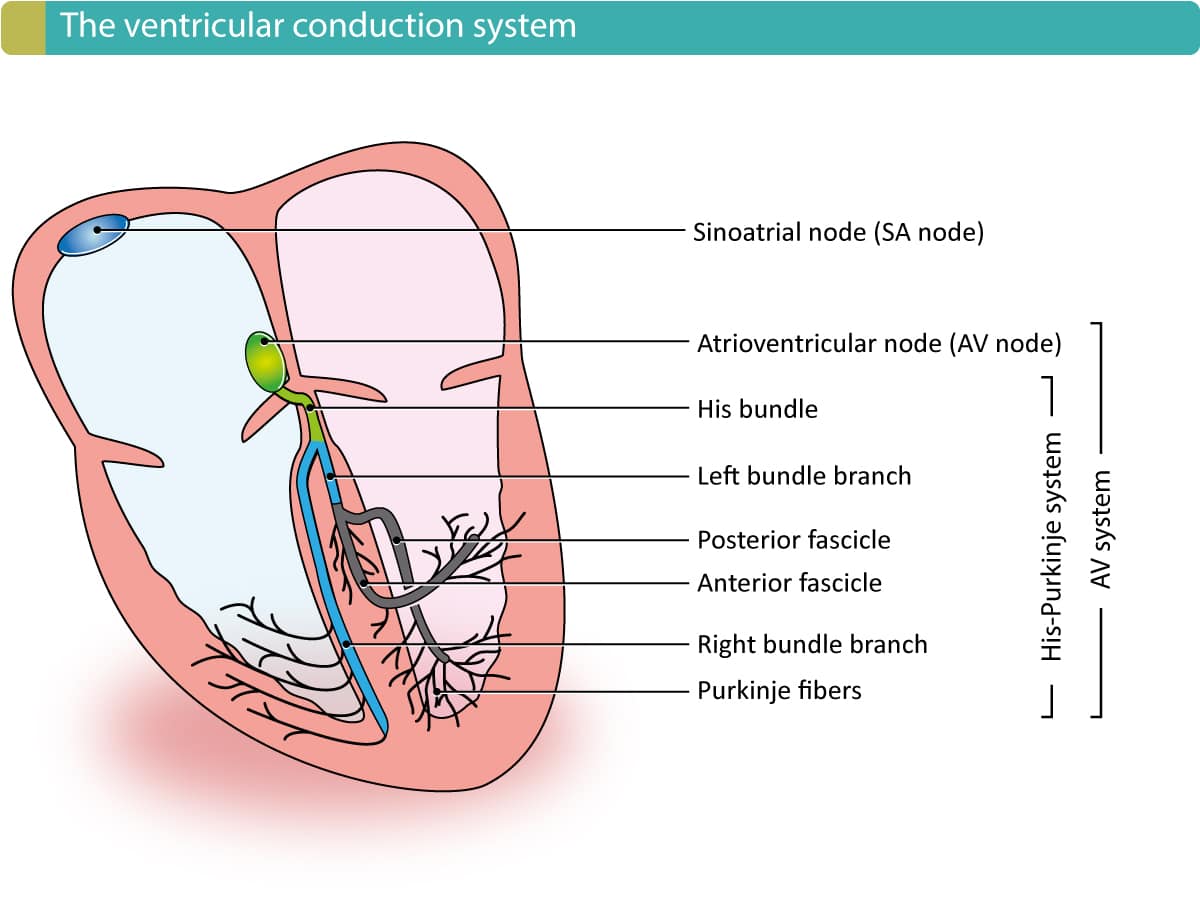
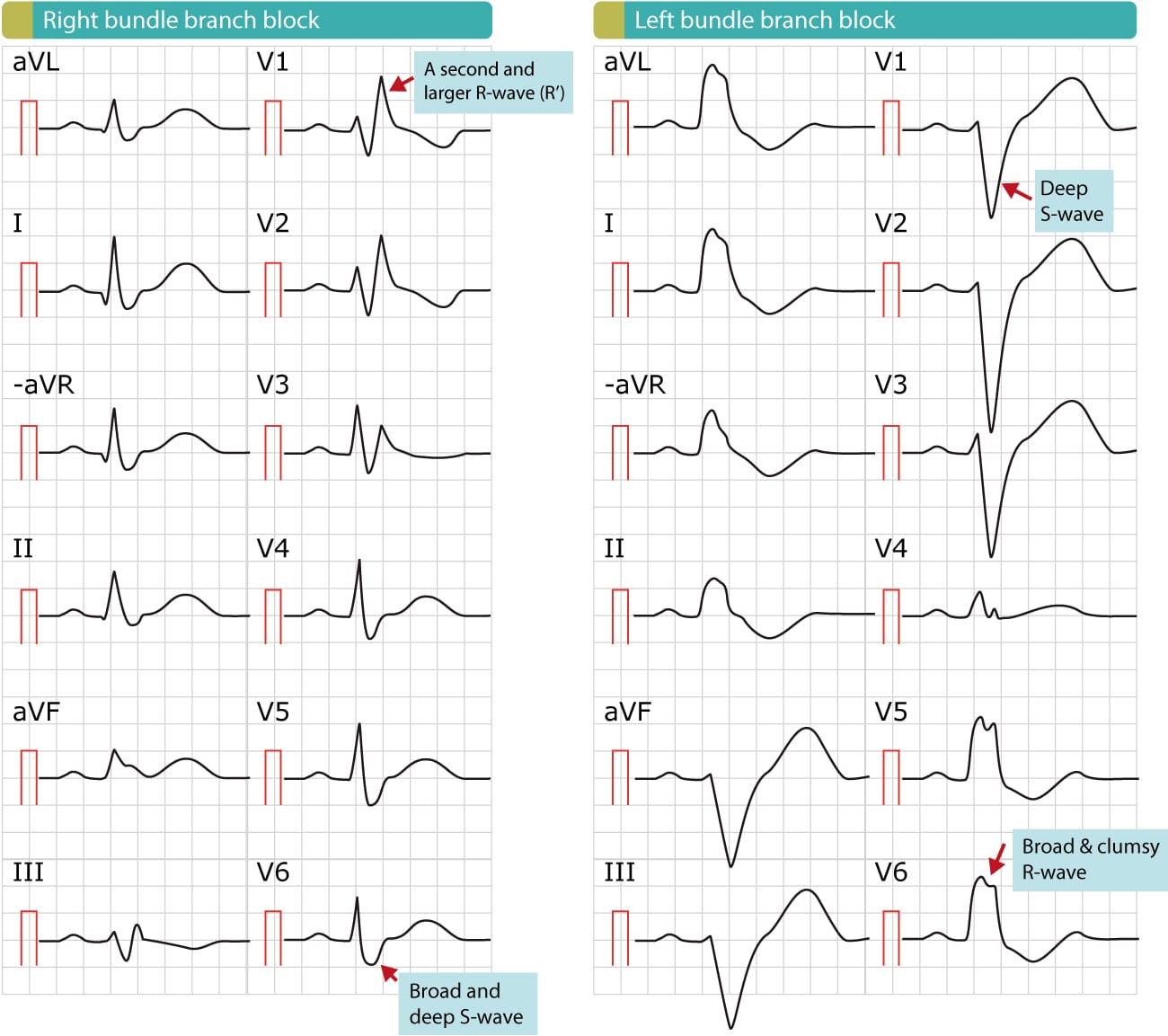
Right bundle branch block (RBBB) is due to an anatomical or functional dysfunction in the right bundle branch, such that the electrical impulse is blocked. Refer to Figure 1 for an overview of the components of the ventricular conduction system, including the right bundle branch. In the setting of RBBB, depolarization (i.e activation) of the right ventricle will depend on electrical impulses spreading from the left ventricle. However, the electrical impulse that spreads from the left ventricle (to the right ventricle) will spread slowly because it travels partly or entirely outside of the conduction system. The slow spread of the impulse will result in a slow (and abnormal) activation of the right ventricle, which yields a bizarre and prolonged QRS complex on ECG. The hallmark of right bundle branch block is QRS duration ≥0,12 seconds, large R’-wave in V1/V2 and a broad and deep S-wave in V5/V6. Figure 2 illustrates a normal ECG, a right bundle branch block (RBBB) and a left bundle branch block (LBBB).
ECG criteria for right bundle branch block (RBBB)
- QRS duration ≥0,12 seconds.
- Leads V1-V2: The QRS complex appears as the letter “M”. More specifically, the QRS complex displays rsr’, rsR’ or rSR’ pattern (rSR’ is the most common, exemplified in Figure 1). Occasionally the S-wave does not reach the baseline. The second R-wave (denoted R’) is virtually always larger than the first R-wave.
- Leads V5, V6, I, aVL: Broad S-wave. S-wave duration is greater than R-wave duration, or S-wave duration is greater than 40 ms in V6 and I.
- ST-T changes: V1-V2 shows downsloping ST-segments and inverted T-waves. Leads V5, V6, I and aVL show positive T-waves.
If the QRS duration is ≥0,110 seconds but <0,12 seconds, the right bundle branch block is said to be incomplete. Note that a second r-wave (r’) may occur as a normal variant in lead V1 (the normal variant has a normal QRS duration). Moreover, the normal septal q-waves (seen in V5, V6) are not affected by right bundle branch block. Occasionally the right bundle branch block only displays a broad and notched R-wave in V1 (instead of two R-waves); in that scenario, the R-wave peak time should be >0.05 seconds.
Electrophysiology of right bundle branch block (RBBB)
Under normal circumstances, both ventricles are depolarized simultaneously, but the ECG is dominated totally by electrical vectors generated by the left ventricle because its muscle mass is substantially larger than the right ventricle. However, in right bundle branch block, the right ventricle is depolarized after the left ventricle, and therefore its electrical vectors may come to expression. The electrical vector of the right ventricle appears on the later part of the QRS complex, in the form of R’-wave (the vector yielding R’ is directed anteriorly and rightward).
Because depolarization of the right ventricle is abnormal, repolarization will also be abnormal. Such repolarization abnormalities are termed secondary ST-T changes. This manifests on the ECG as discordant ST-T segments, meaning that the ST-T segment is directed oppositely to the QRS complex. As shown in Figure 1, the positive QRS complex in V1 is followed by a negative ST-T segment with ST-segment depression and T-wave inversion. Similar changes are typically seen in V2.
The right bundle branch block does not alter the electrical axis of the heart. Axis deviation indicates that there is a concomitant fascicular block. Left axis deviation suggests concomitant left anterior fascicular block. Right axis deviation suggests concomitant left posterior fascicular block.
Clinical significance of right bundle branch block
Right bundle branch block in asymptomatic individuals is not correlated with adverse outcomes. On the other hand, a new right bundle branch block in patients with chest pain may indicate occlusion in the left anterior descending artery. Finally, a new right bundle branch block in patients experiencing dyspnea (particularly if acute) may indicate pulmonary embolism. In the vast majority of cases, however, right bundle branch block is a benign finding with little if any impact on cardiovascular prognosis. Young individuals rarely display right bundle branch block. However, incomplete right bundle branch block occurs occasionally even in younger persons. A large prospective cohort study evaluated the association between right bundle branch block and mortality over a period of 20 years in otherwise healthy individuals; no association was found.
Causes of right bundle branch block (RBBB)
- Idiopathic fibrosis or degeneration in the right bundle branch
- Congenital heart disease
- Ischemic heart disease (coronary artery disease)
- Acute cor pulmonale (pulmonary embolism)
- Chronic obstructive pulmonary disease
- Cardiac surgery may cause permanent or transient RBBB
- PCI may cause transient RBBB
- Cardiomyopathy (particularly hypertrophic obstructive cardiomyopathy) may cause RBBB
- Aberrant ventricular conduction (aberrancy)
Diagnosis of ischemia and infarction in the setting of RBBB
The right bundle branch block does not interfere with the diagnosis of ischemia/infarction. It is possible to diagnose pathological Q-waves (because the initial part of the QRS is not affected by the RBBB). Acute ischemia (ST-T changes) may also be judged as usual, despite the bundle branch block. Note that acute cor pulmonale with RBBB may cause large Q-waves in V1–V3, II, III and/or aVF.
 Next chapter
Next chapter
Left bundle branch block (LBBB): ECG, criteria, causes & management
 Related chapters
Related chapters
Overview of Intraventricular Conduction Defects
Nonspecific intraventricular conduction delay
View all chapters in Supraventricular and Intraventricular Conduction Defects

 Next chapter
Next chapter Related chapters
Related chapters