Aberrant ventricular conduction (aberrancy, aberration)
Aberrant ventricular conduction (aberrancy, aberration)
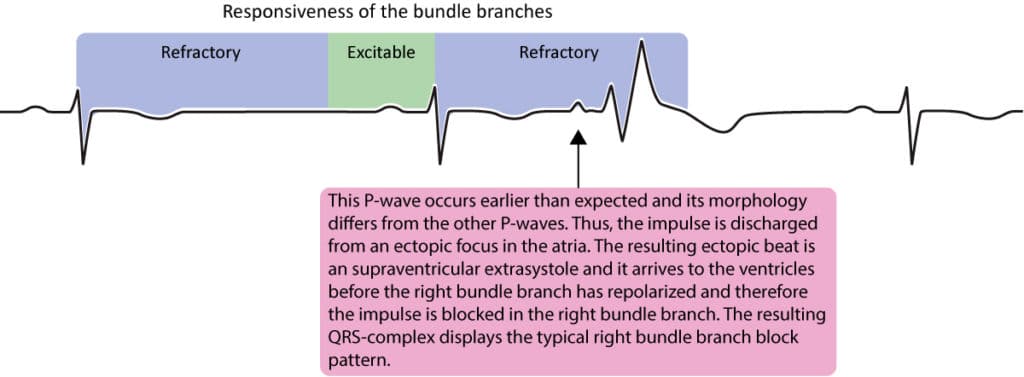
Aberrant conduction is not a mechanism of arrhythmia; it is a ventricular conduction disturbance. It is discussed in this chapter because the phenomenon is frequently observed during arrhythmias. As previously discussed, all cardiac cells—both conduction and contractile cells—must undergo rapid repolarization to ensure they are excitable when the next action potential occurs. If any component of the ventricular conduction system has not fully repolarized by the time the next impulse reaches the ventricles, the impulse will be blocked at that point. The length of the refractory period (see Basic Cardiac Electrophysiology) varies with heart rate. The length is shortened as heart rate increases and vice versa. Thus, long cycles (i.e. long RR intervals) are associated with long refractory periods and short RR intervals have shorter refractory periods. Aberrant conduction occurs when the length of the cardiac cycle is changed without a compensatory change in the length of the refractory period. This is explained by the changes in the refractoriness in the His-Purkinje system related to changes in the RR interval.
Figure 1 shows a premature atrial beat causing aberrant ventricular conduction. A premature atrial beat is simply an extra (unexpected) beat discharged by an ectopic focus in the atria. The impulse from the premature beat reaches the His-Purkinje system early, while some fibers are still refractory. In this case (Figure 1) it encounters a refractory right bundle branch and therefore the impulse is conducted with right bundle branch block morphology. This is an example of how changes in the length of the cardiac cycle causes aberration.
In clinical practice aberration is commonly seen in patients with atrial fibrillation because these patients have rapid and irregular rhythms with frequently changing RR intervals. Refer to Figure 2.
Aberrancy can occur in three different situations, all related to changes in cardiac cycle length. These situations are as follows:
- Premature ventricular depolarization: As exemplified in Figure 1, if the atrial impulse reaches the ventricular His-Purkinje system too early – while conduction fibers are still refractory – the impulse might be blocked. This is a frequent finding among healthy individuals and in those with heart disease. If such aberration occurs at normal heart rate (<100 beats/min) it is most likely to have a right bundle branch block morphology. If the aberration occurs during higher heart rates, it is more likely that the QRS complex will have a left bundle branch block morphology. However, left bundle branch block morphology is more common (regardless of heart rate) among persons with heart disease. Alternating block (right and left bundle branch block alternating from one beat to another) is uncommon.
- Ashman’s phenomenon: This type of aberration occurs when the RR interval is first prolonged and then shortened. The initial prolongation increases the length of the refractory period and the subsequent early impulse will therefore encounter refractory fibers. Thus, Ashman’s phenomenon requires a long RR interval followed by a short RR interval (Figure 2). These aberrantly conducted beats typically have right bundle branch block morphology.
- Sudden acceleration in heart rate: If the heart rate accelerates suddenly, the bundle branches may not be able to accommodate (i.e shorten) their refractory periods appropriately. The aberration may persist if the heart rate stabilizes at a high rate, but it usually resolves as the His-Purkinje system manages to adapt its refractory period. If the acceleration occurs at low heart rates, the aberrantly conducted beat will exhibit right bundle branch morphology. If the rate accelerates at higher heart rates, it will typically exhibit a left bundle branch block morphology.
The majority of all aberrantly conducted beats have right bundle branch block morphology. This is due to the longer refractory period of the right bundle branch at normal heart rates. Aberration may also occur in either of the fascicles (anterior or posterior fascicle of the left bundle branch). Left bundle branch morphology at normal heart rate suggests underlying heart disease.
Differentiating aberration from premature ventricular complexes
Aberrantly conducted beats may be difficult to differentiate from premature ventricular beats but it is mostly possible to differentiate these entities. In Figure 1 a P-wave is visible before the aberrantly conducted beat and this assures a supraventricular origin of the impulse and the wide QRS complex is therefore due to aberration. Premature ventricular complexes are not preceded by P-waves (other than by randomness). Premature ventricular complexes are, however, more common than aberrantly conducted beats. Aberrantly conducted beats display typical bundle branch block morphology, which premature ventricular complexes do not. Aberrantly conducted beats are not followed by a full compensatory pause (discussed later), which premature ventricular beats are.

