ST segment depression in myocardial ischemia and differential diagnoses
ST segment depression due to acute myocardial ischemia
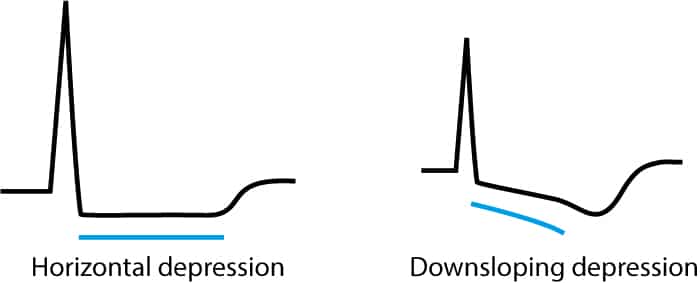
ST segment depressions caused by ischemia are characterized by a horizontal or downsloping ST segment. Indeed, North American and European guidelines assert that the ST segment must be either downsloping or horizontal. Otherwise, ischemia is unlikely to be the cause of the ST segment depression. The horizontal ST segment depression is more specific than the downsloping depression. Refer to Figure 1.
Current guideline criteria for ischemic ST segment depression:
New horizontal or downsloping ST segment depressions ≥0,5 mm in at least two anatomically contiguous leads.
The transition from ST segment to T-wave is more abrupt in ischemia (the transition is normally smooth). Refer to Figure 2.

Ischemic ST segment depressions occur in both NSTE-ACS (NSTEMI and unstable angina pectoris) and STE-ACS (STEM). However, the significance of the ST segment depression differs markedly in NSTE-ACS and STE-ACS. In NSTE-ACS the ST segment depressions are the primary ischemic ECG changes. ST segment depressions in NSTE-ACS are frequently accompanied by T-wave inversions (or flat T-waves), but the primary ECG finding is the ST segment depressions. In STE-ACS, on the other hand, the ST segment depressions are secondary findings and the primary findings are the ST segment elevations. As explained in the previous article, ST segment depressions in STE-ACS are actually reciprocal (mirror images) to ST segment elevations.
ST segment depressions with upsloping ST segment are rarely caused by ischemia, with one notable exception. Occurrence of upsloping ST segment depressions with prominent T-waves in the majority of the chest leads may indicate an acute occlusion in the LAD (left anterior descending artery). This ECG pattern is referred to as de Winter’s ECG.
Figure 3 provides all clinically relevant differential diagnoses, and their ECG appearance, to ischemic ECG changes. This figure must be studied carefully.

Differential diagnoses in ST segment depressions
Please refer to Figure 3 for examples.
Normal (physiological) ST segment depressions
Normal (physiological) ST segment depressions occur during physical exercise. These ST segment depressions have an upsloping ST segment. The depression in the J 60 point is usually <1 mm and it resolves rapidly once the exercise is stopped. Some experts believe that these ST segment depressions represent a benign form of subendocardial ischemia. Refer to Exercise Stress Testing for details.
Hyperventilation
Hyperventilation causes ST segment depressions very similar to those normally seen during physical exercise.
Left ventricular hypertrophy (LVH), right ventricular hypertrophy (RVH), left bundle branch block (LBBB), right bundle branch block (RBBB) and pre-excitation
Left ventricular hypertrophy (LVH), right ventricular hypertrophy (RVH), left bundle branch block (LBBB), right bundle branch block (RBBB) and pre-excitation (WPW syndrome) may all cause ST segment depressions. These are all common conditions in which an abnormal depolarization (QRS complex) causes abnormalities in the repolarization (ST-T-segment). For example, a block in the left bundle branch (i.e left bundle branch block) means that the left ventricle will not be depolarized via the Purkinje network, but rather via spread of the depolarization from the right ventricle. The abnormal ventricular depolarization will cause an abnormal repolarization. For this reason, these ST-T changes are referred to as secondary ST-T changes. It is actually expected that these conditions display such secondary ST-T changes; the absence of such changes should lead to suspicion of ischemia (if the patient has symptoms consistent with ischemia). The same is true for artificial pacemakers (virtually all pacemakers stimulate the ventricles in the right ventricular apex). Thus, it is expected to observe secondary ST-T changes during pacemaker rhythm.
Digoxin
Digoxin (digitalis, digitoxin) causes downsloping ST depression with a characteristic “sagging” appearance.
Sympathetic stimulation and hypokalemia
Sympathetic stimulation and hypokalemia cause non-specific ST segment changes.
Heart failure
Heart failure may cause ST segment depressions in left-sided leads (V5, V6, I and aVL). These depressions are horizontal or downsloping.
Supraventricular tachycardia
Supraventricular tachycardia may also cause ST segment depressions. These depressions are usually horizontal or upsloping and tend to be most evident in leads V4–V6. these ST segment depressions resolve rapidly once the tachycardia has resolved.
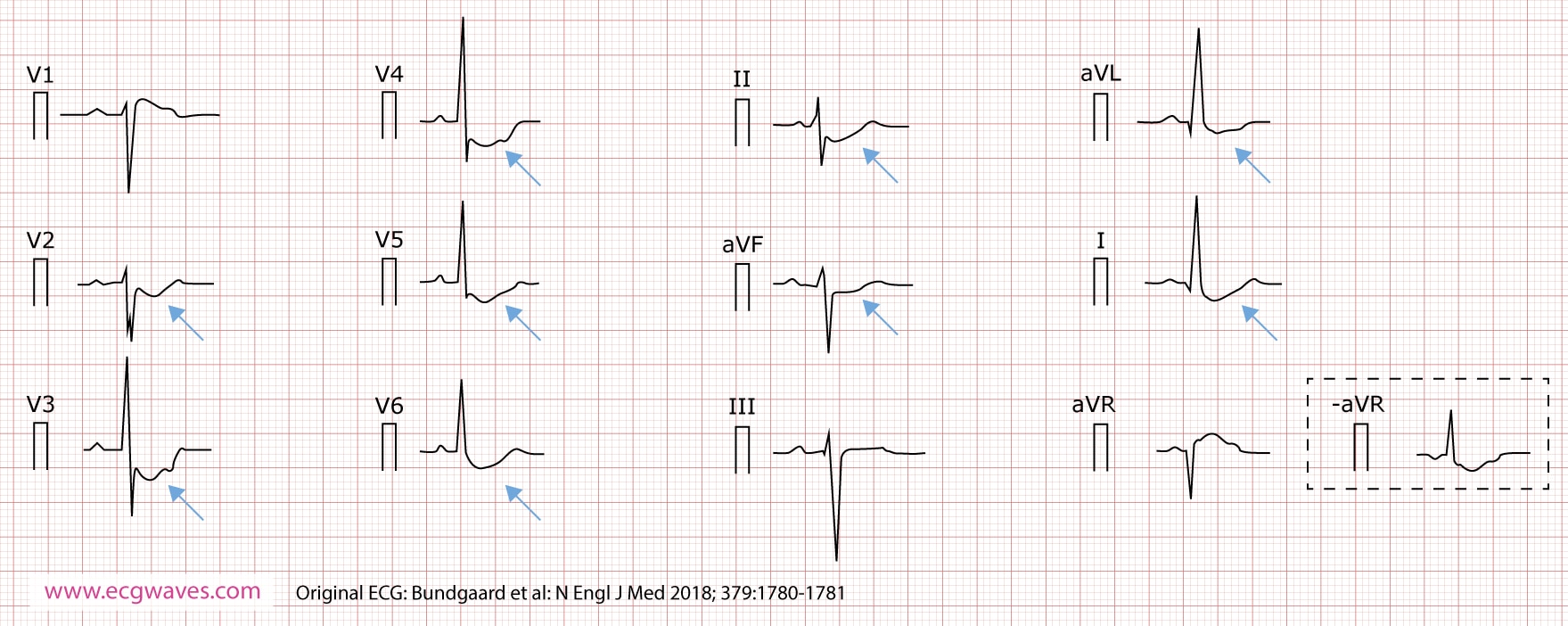
A novel cardiac syndrome with concave-upward ST-segment depressions
In November 2018 researchers from Denmark, Netherlands and United Kingdom reported a novel ECG syndrome characterized by widespread ST-segment depressions and an increased risk of sudden cardiac arrest. The researchers identified five unrelated families with features that represent a previously unrecognized autosomal dominant syndrome (Figure 4). The ECG is characterized by deep and persistent, concave-upward ST-segment depression in multiple limb and chest leads. ECG changes are stable over time and accentuated during exercise. Patients present with syncopal episodes, ventricular tachycardia (including torsade de pointes), ventricular fibrillation and sudden cardiac arrest.