Ventricular fibrillation, pulseless electrical activity and sudden cardiac arrest
Ventricular fibrillation, pulseless electrical activity (PEA) and sudden cardiac arrest
This chapter will focus on ventricular fibrillation and pulseless electrical activity (PEA). These are highly lethal arrhythmias that lead to death if cardiopulmonary resuscitation is not started immediately. Ventricular fibrillation is the result of numerous re-entry circuits, causing rapid and chaotic ventricular depolarizations, rendering the left ventricle incapable of generating effective contractions. This results in circulatory collapse, loss of consciousness, and sudden cardiac arrest. Unlike ventricular tachycardia, ventricular fibrillation seldom self-terminates and death is imminent without immediate and resuscitative efforts.
Approximately 80% of individuals who suffer a sudden cardiac arrest have ventricular fibrillation prior to the cardiac arrest. Most of these have atherosclerotic heart disease (coronary artery disease) as the underlying cause. Other common causes are cardiomyopathy (hypertrophic or dilated), arrhythmogenic right ventricular cardiomyopathy, Brugada syndrome, early repolarization. Electrolyte disorders, acidosis, hypoxemia and ischemia all aggravate the risk of developing ventricular fibrillation, in any situation.
ECG features of ventricular fibrillation
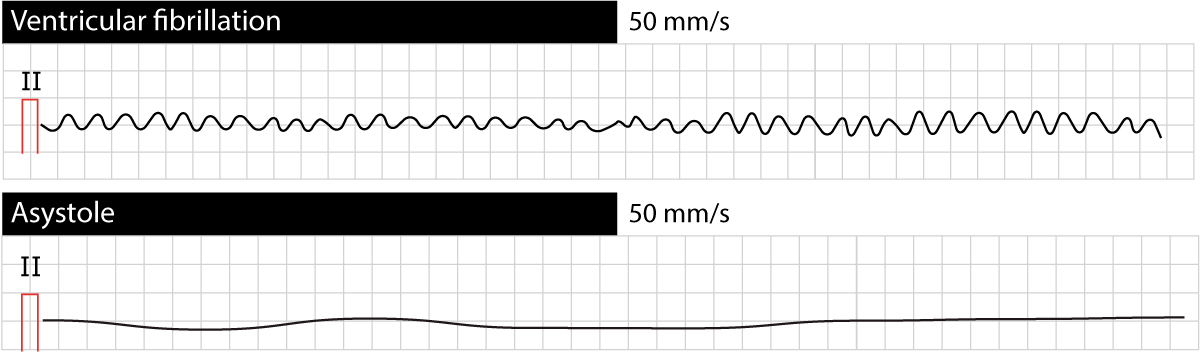
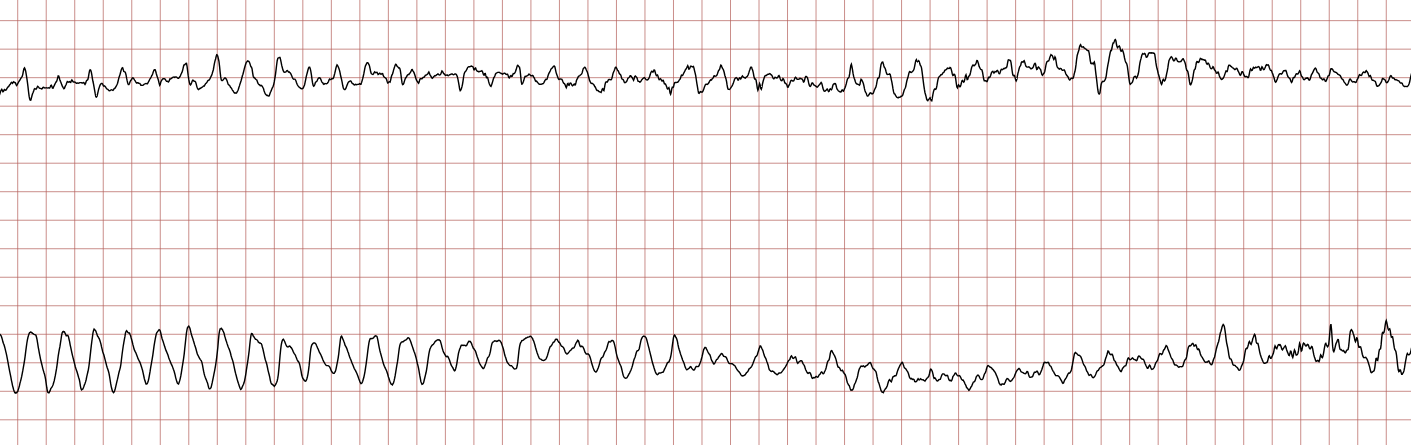
The ECG shows irregular waves with varying morphology and amplitude. No P-wave, QRS complex or T-wave can be seen. This is pathognomonic (unique) to ventricular fibrillation and must not be confused with any other arrhythmia.
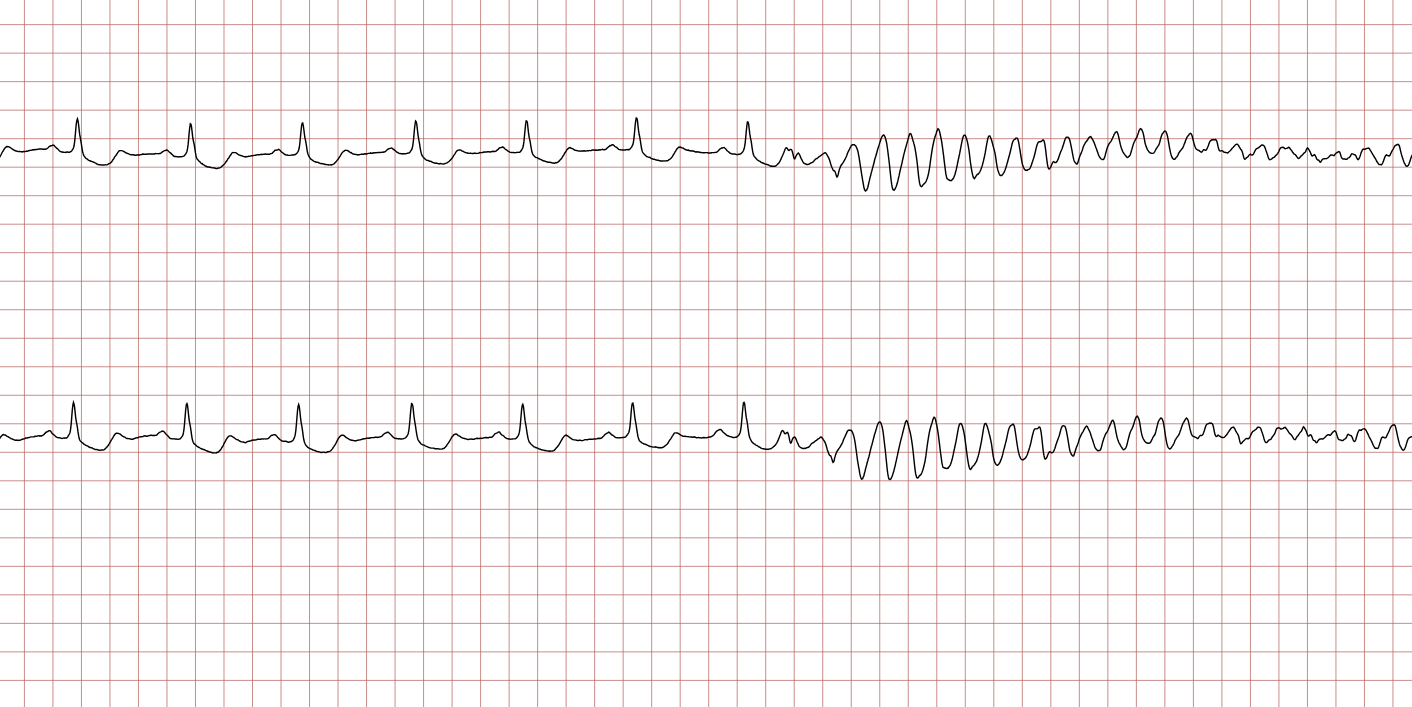
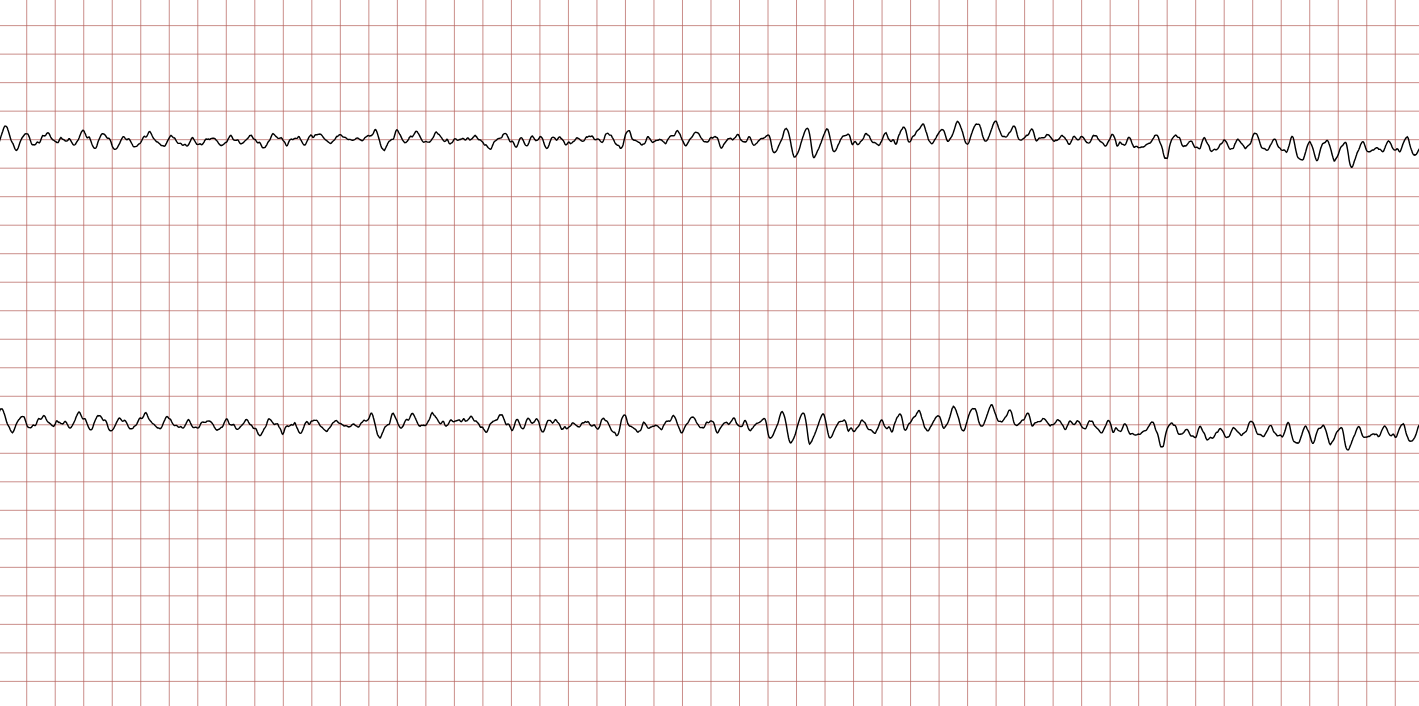
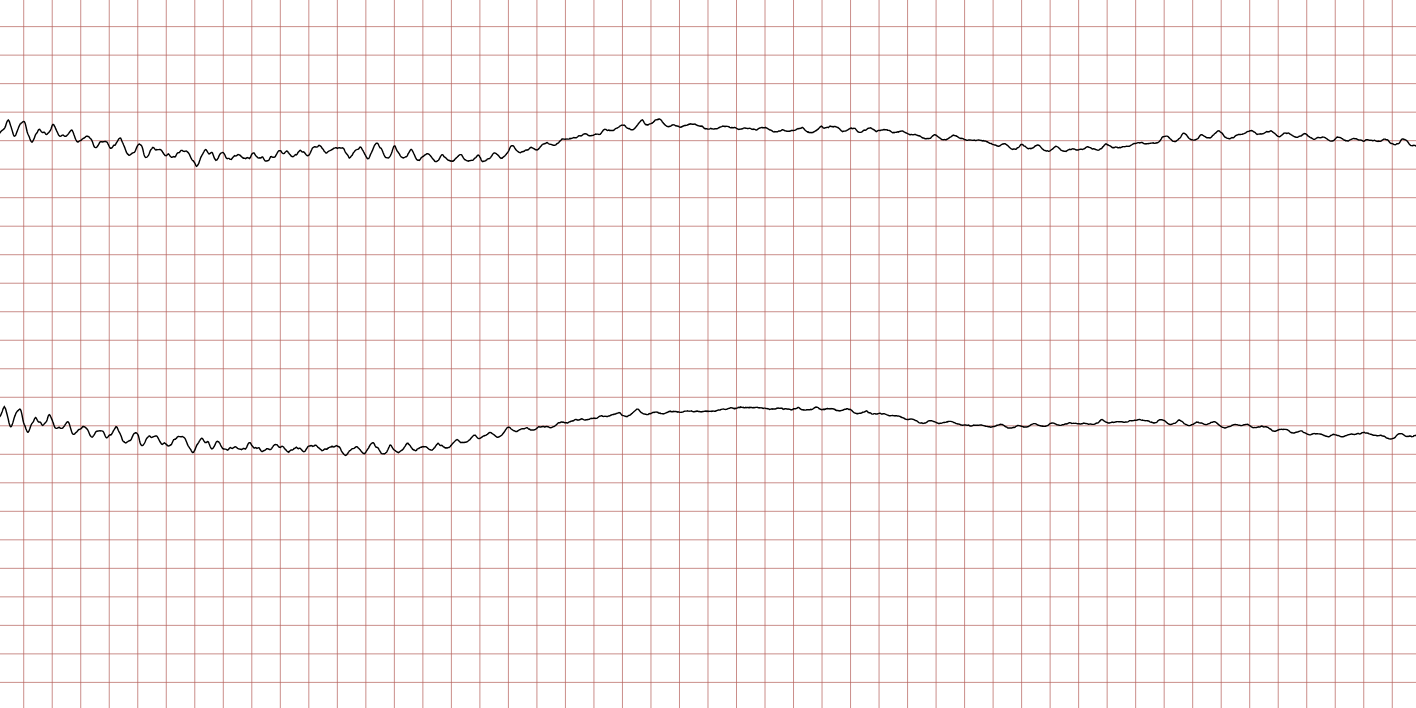
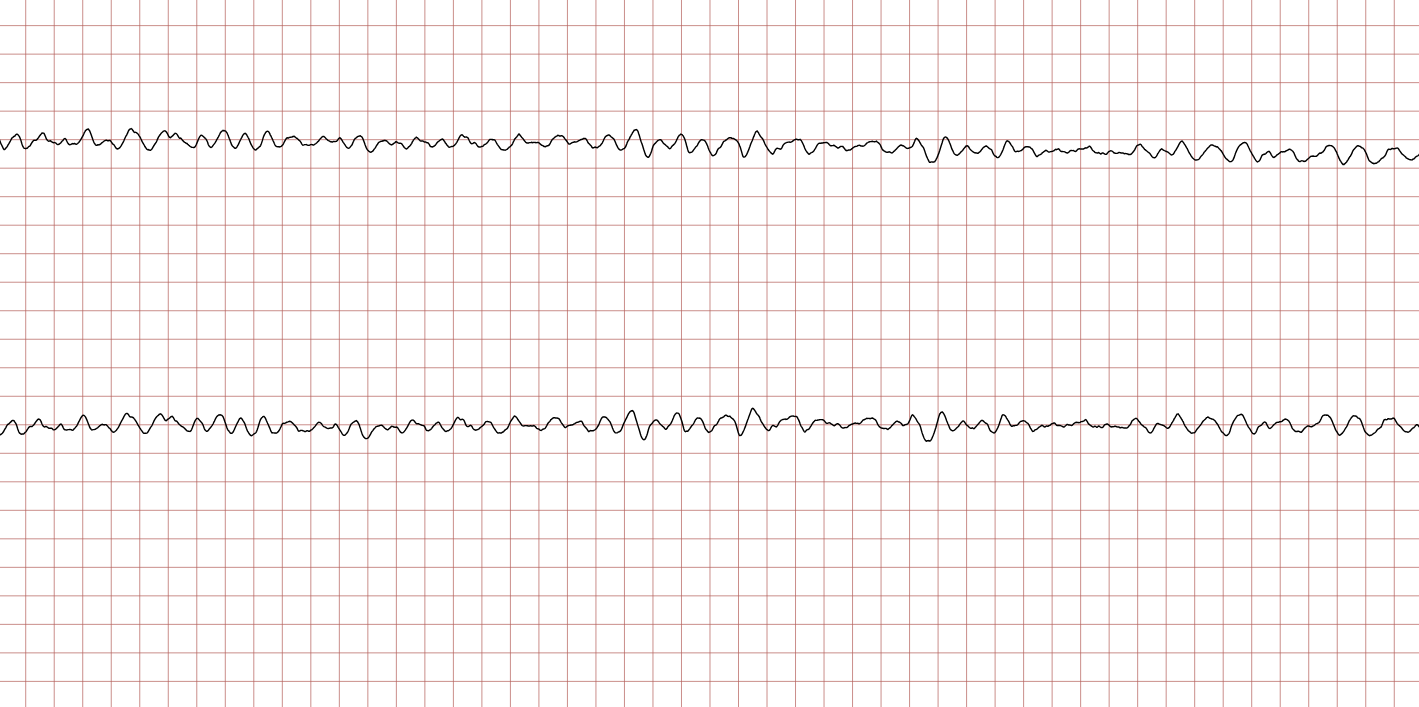
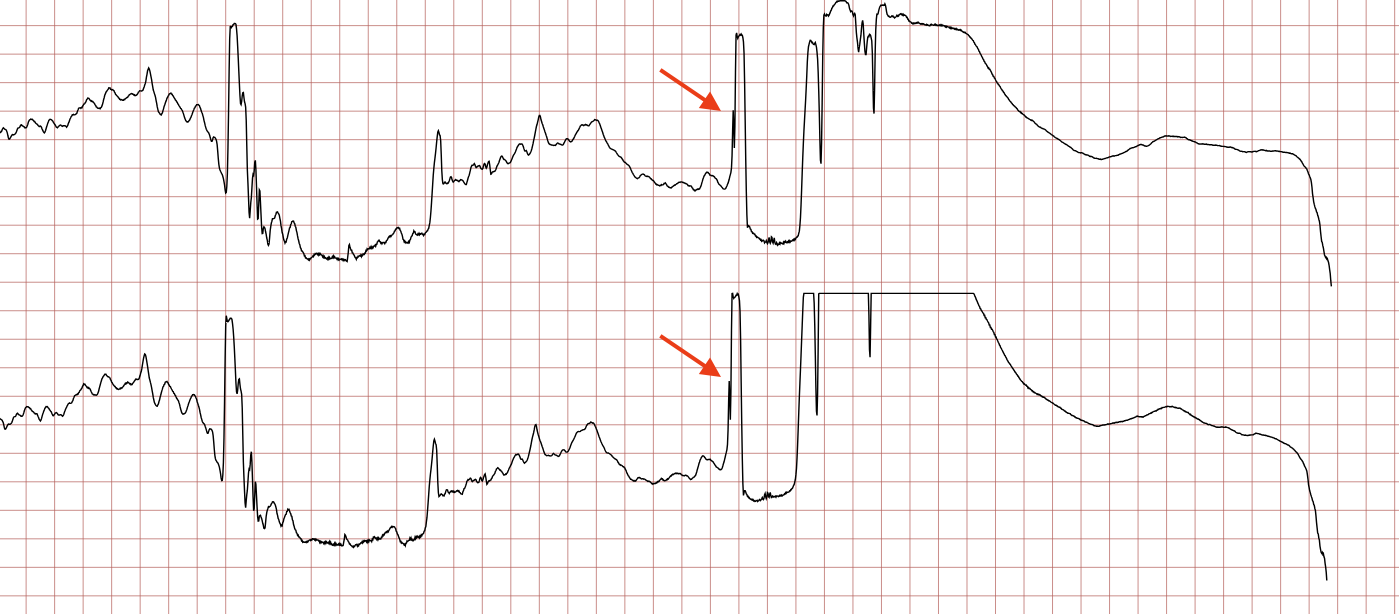
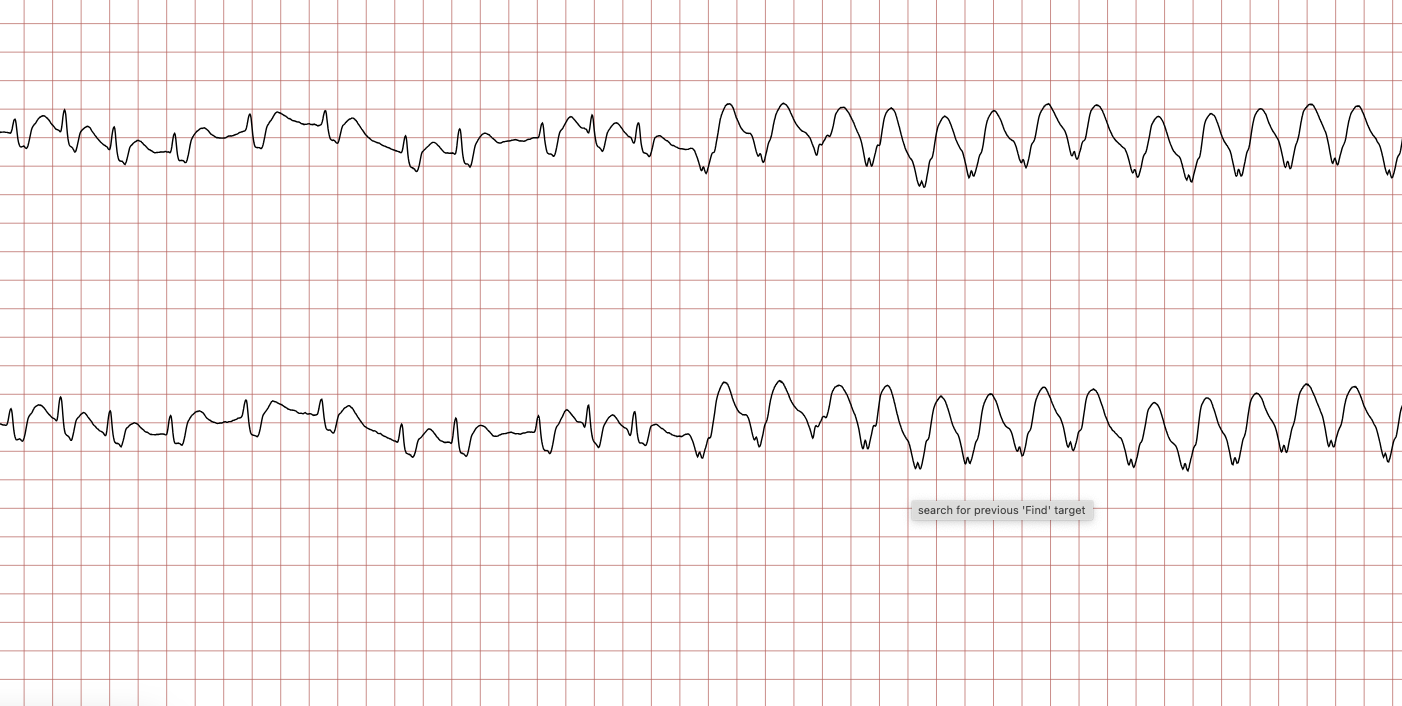
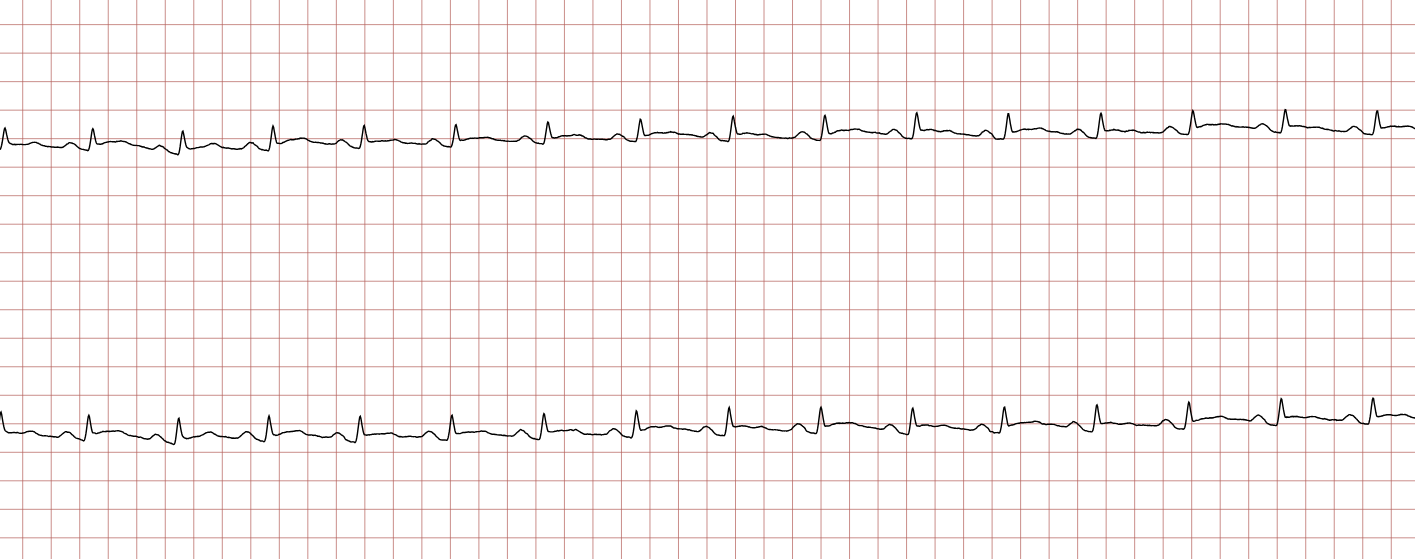
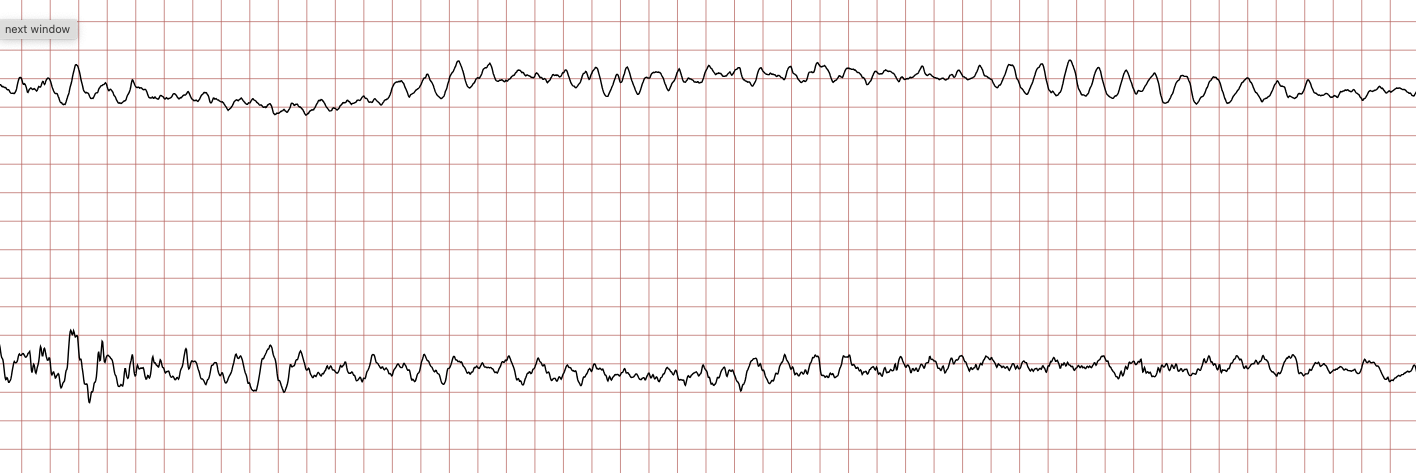
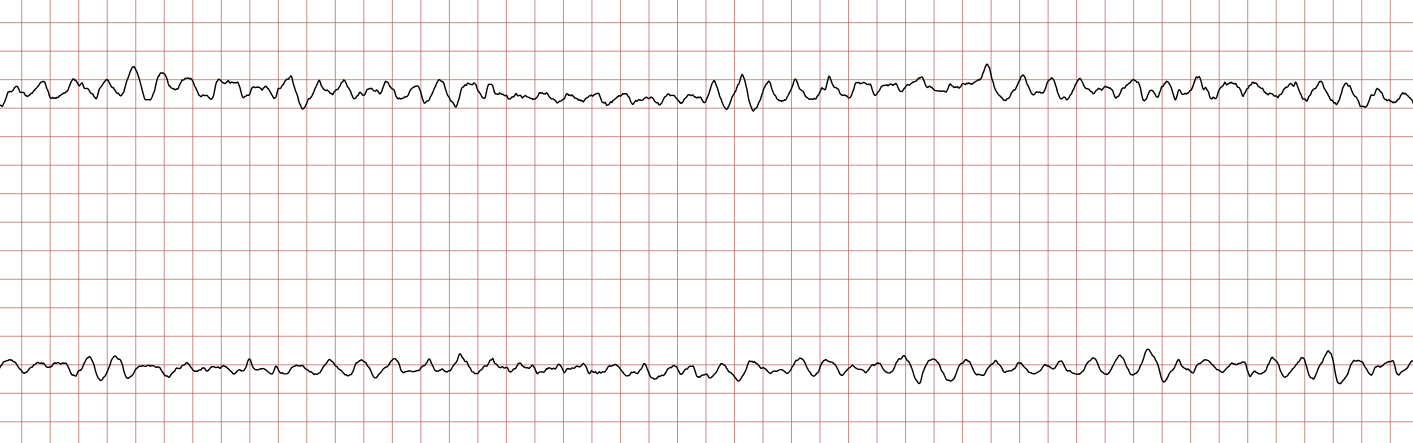
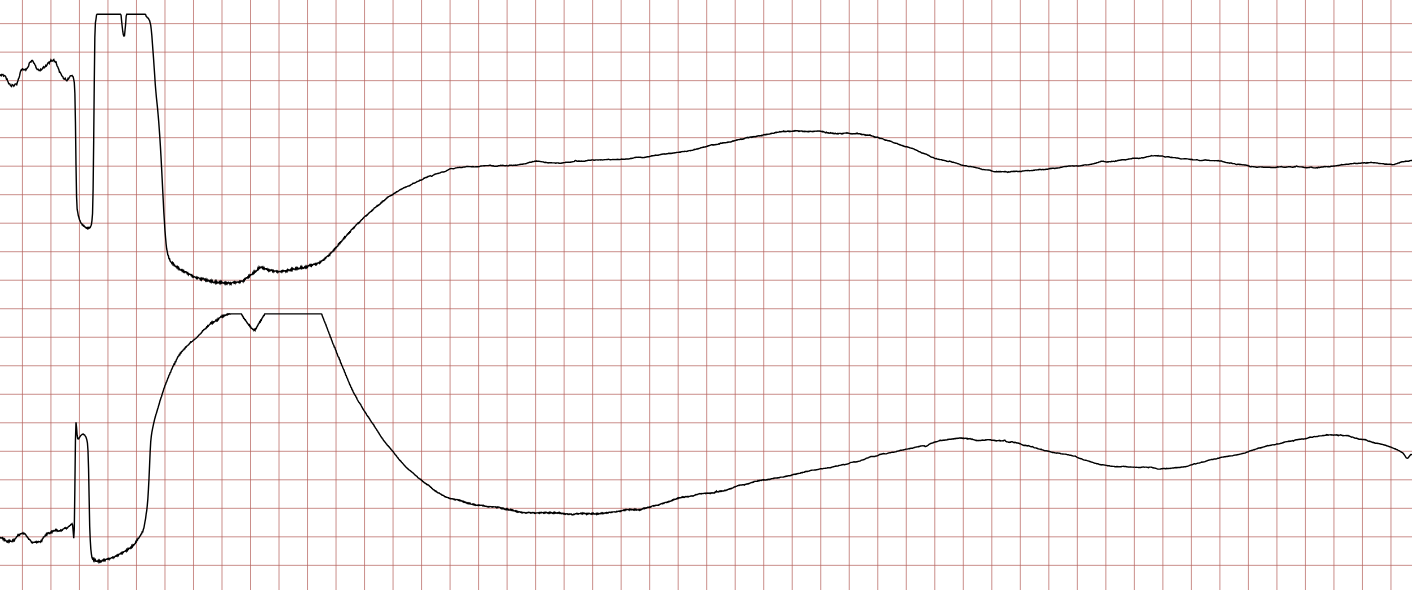
ECG Case 1: Ventricular tachycardia progressing to ventricular fibrillation
Below are sequential ECG recordings during a sudden cardiac arrest in a 43-year-old male. Each ECG presents two leads recorded simultaneously.

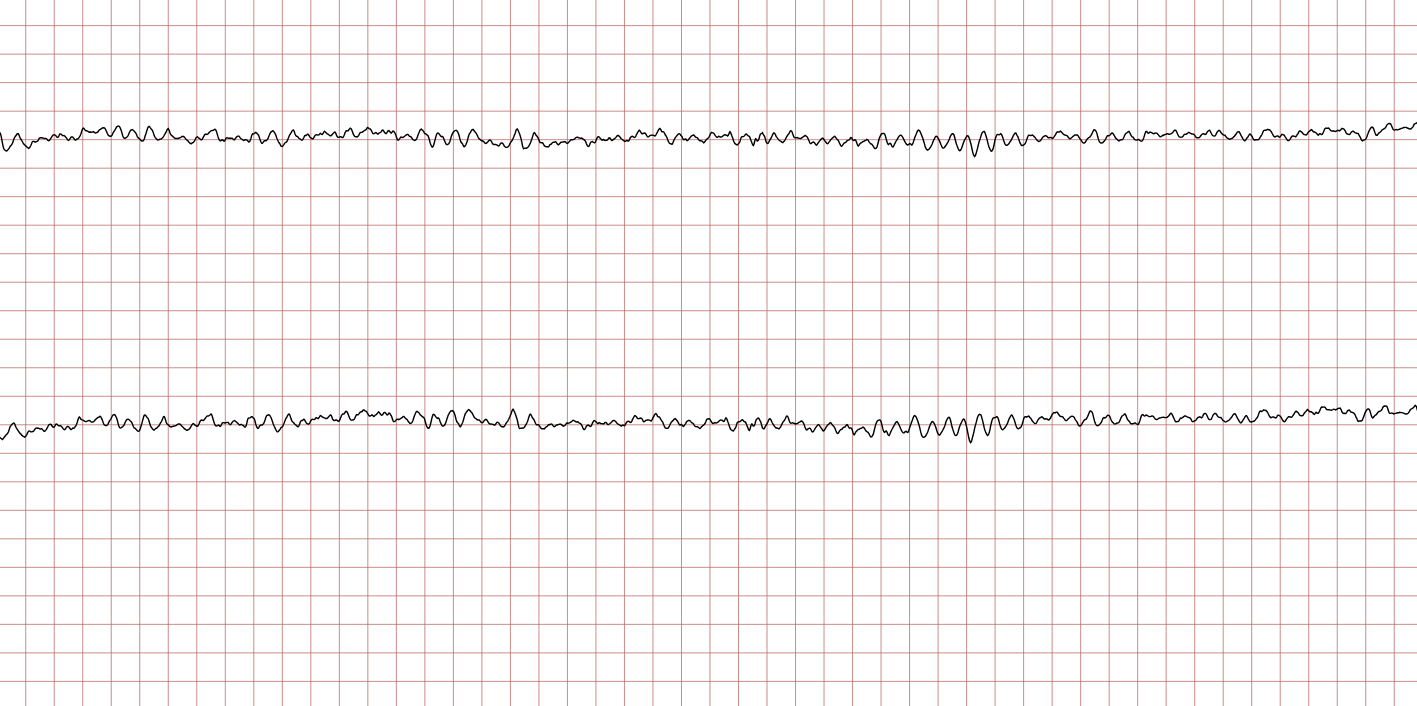
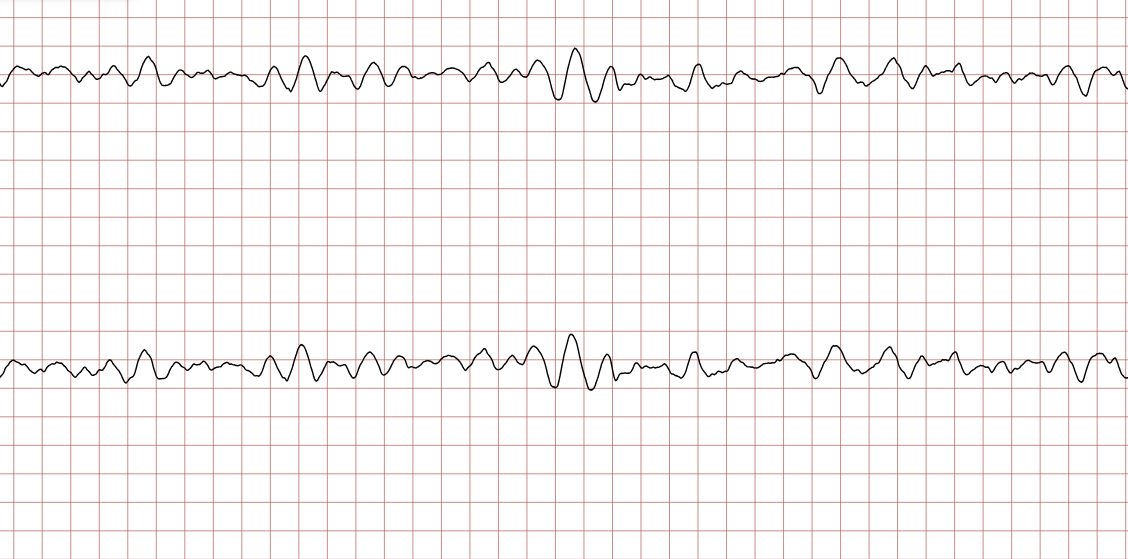
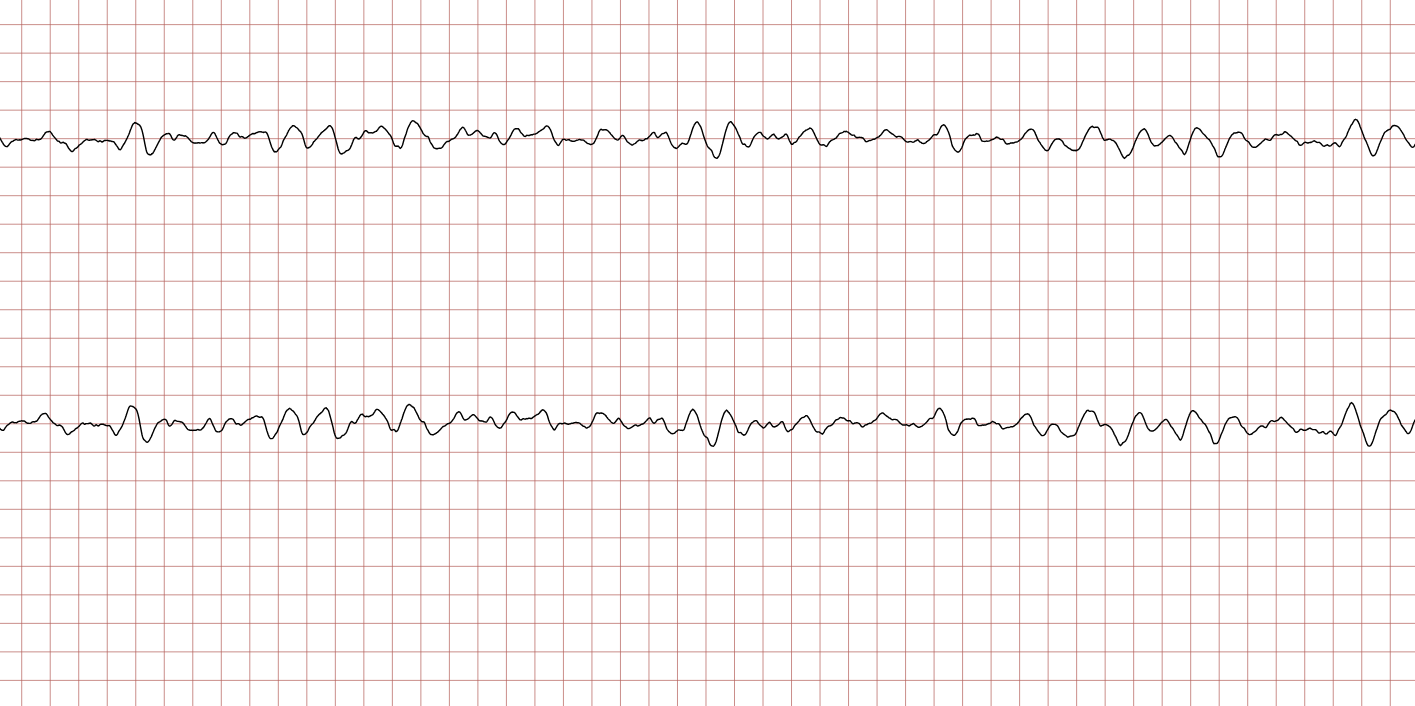
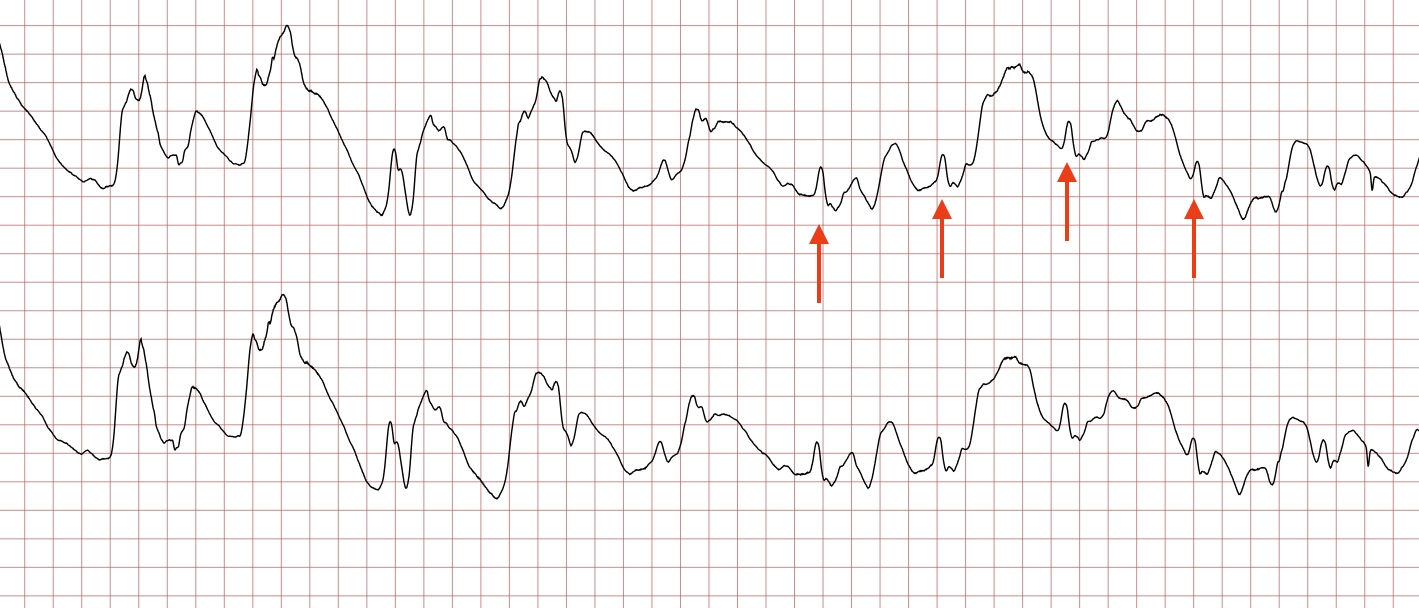
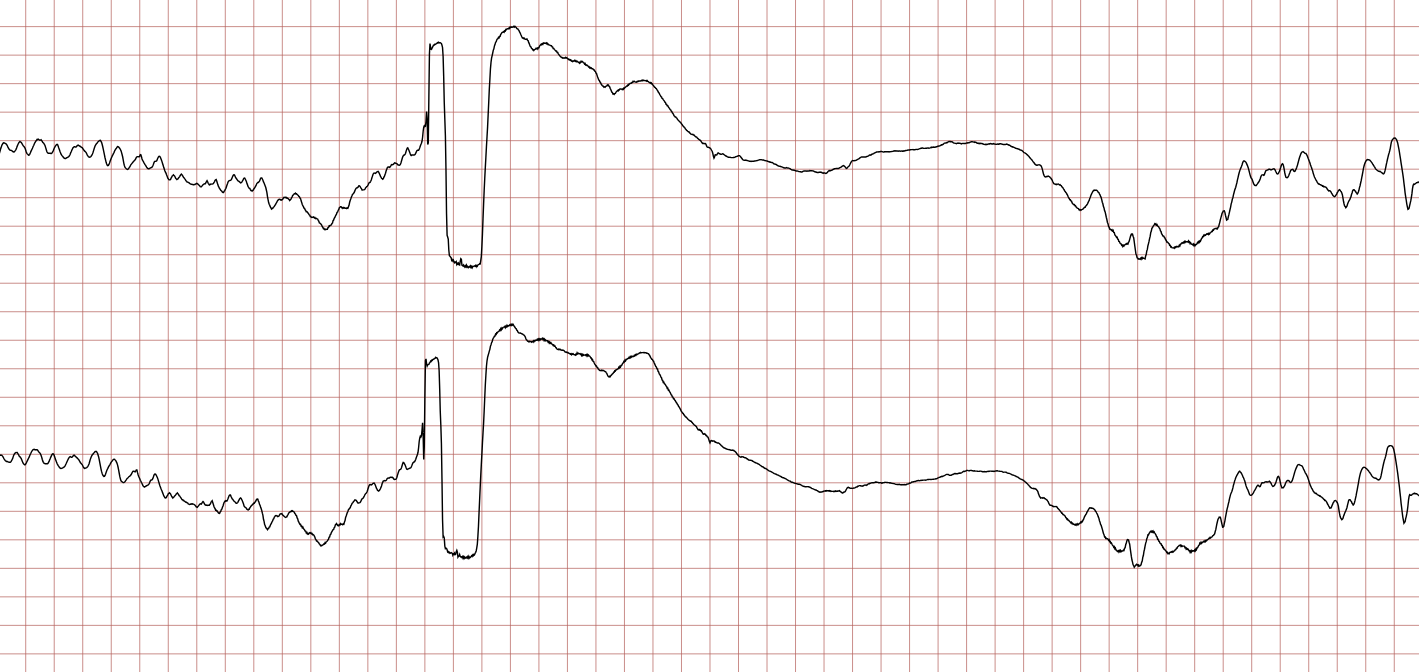
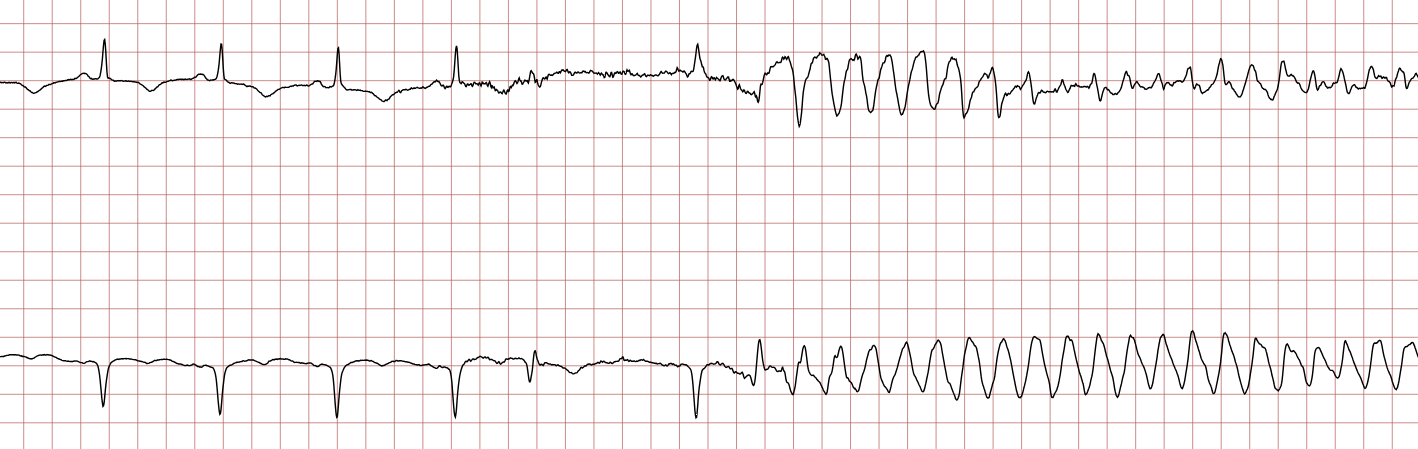
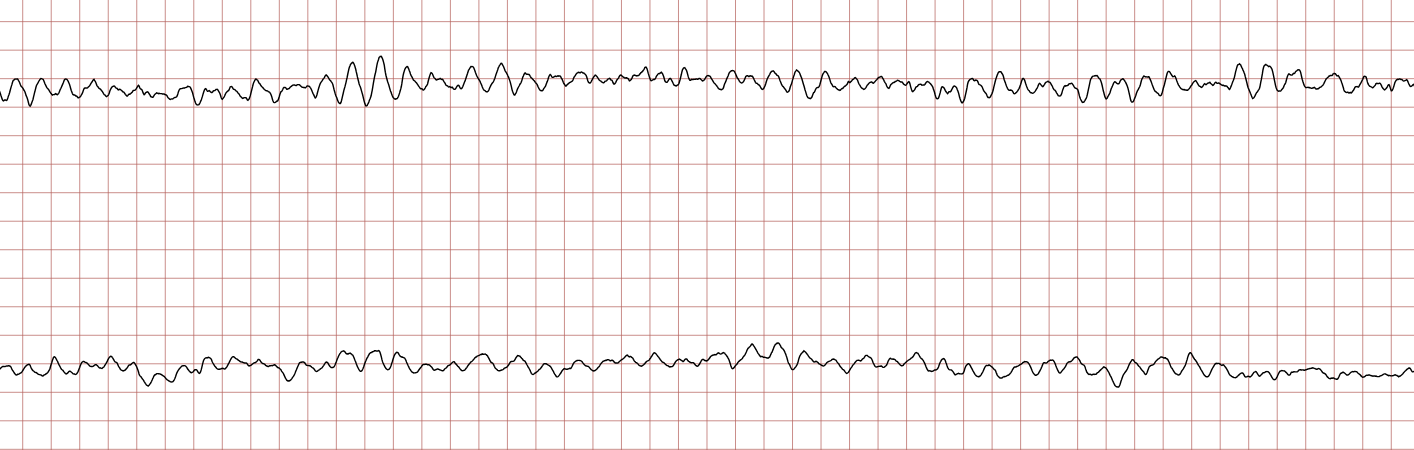
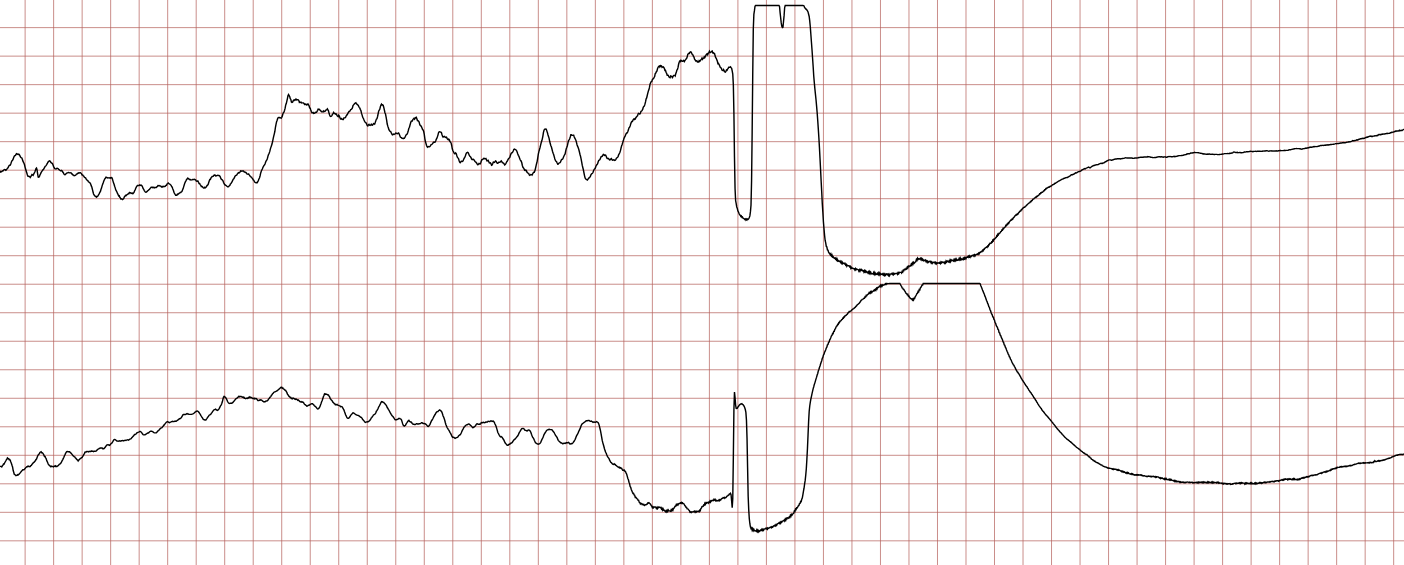
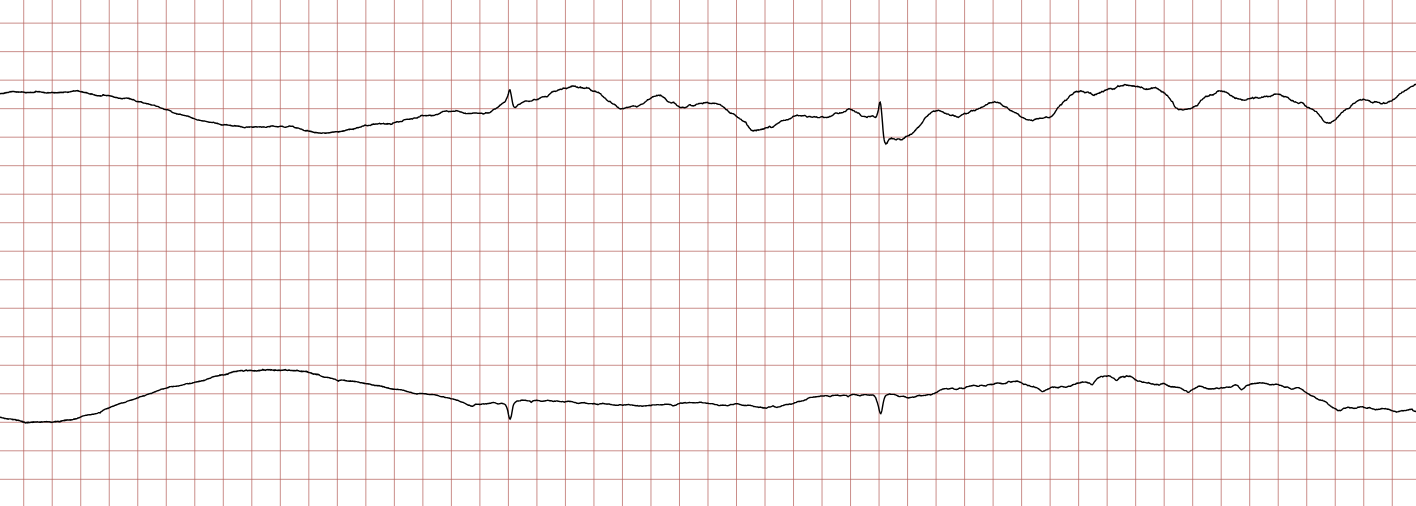
ECG Case 2: Ventricular tachycardia progressing to ventricular fibrillation
Below are sequential ECG recordings during a sudden cardiac arrest in a 62-year-old male. Each ECG presents two leads recorded simultaneously.

Treatment of ventricular fibrillation
Ventricular fibrillation is treated according to the resuscitation algorithm.
Cardiac arrest and sudden cardiac death
For details regarding sudden cardiac arrest and death, please refer to Sudden Cardiac Arrest and Cardiopulmonary Resuscitation (CPR).
Cardiac arrest ensues when ventricular contractions cease or are meaningless. This immediately leads to syncope and soon death, unless resuscitation is attempted. Sudden cardiac death is defined as an unexpected death due to cardiac causes that occur within 1 hour of symptom onset. The person may or may not have known cardiac disease. Moreover, the time limit (1 hour) is not absolute. Sudden cardiac death causes 7 million deaths annually worldwide. The most common cause of sudden cardiac death is acute or chronic coronary artery disease (ischemic heart disease). Cardiomyopathies (dilated or hypertrophic), valvular disease, genetic mutations (LQTS, Brugada syndrome, early repolarization), etc, are much less common than ischemic heart disease.
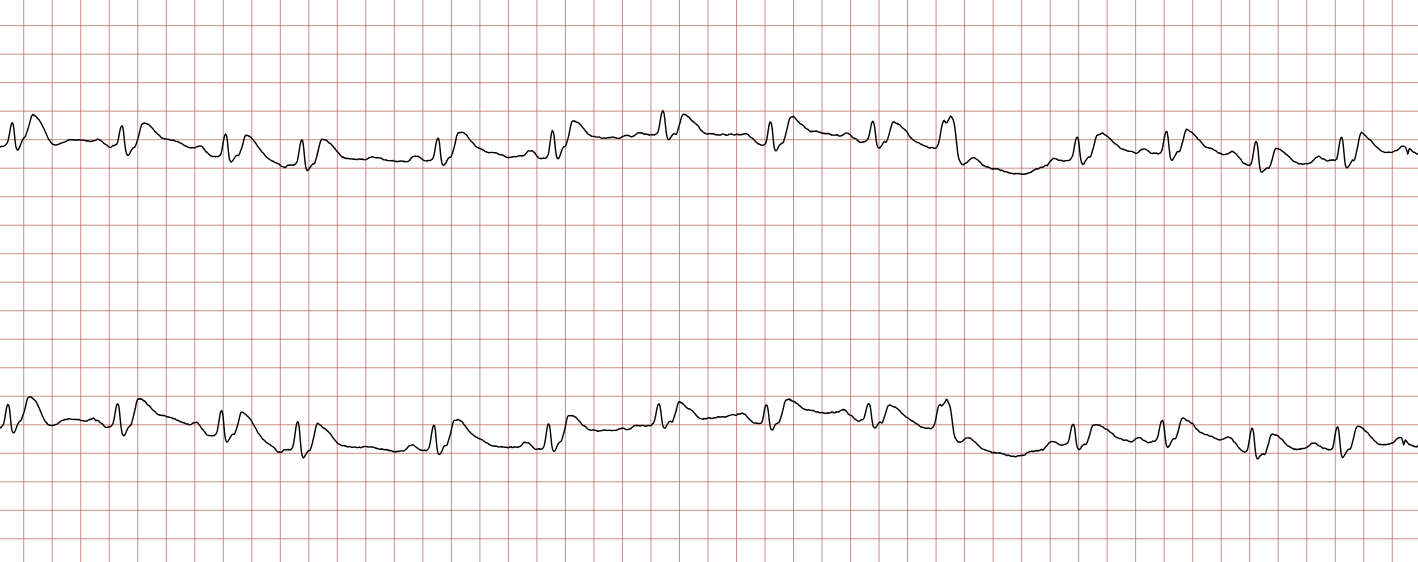
The death mechanism is usually the same regardless of the underlying disease: electrical instability triggers ventricular tachycardia which degenerates into ventricular fibrillation which leads to asystole. The latter, asystole, means that there is no electrical activity in the heart and the ECG shows a flat line (Figure 1). Sudden cardiac death due to bradycardia or pulseless electrical activity is much less common.
Underlying causes
- Acute or chronic ischemic heart disease causes 80% of all sudden cardiac deaths – Ventricular arrhythmias may arise during acute ischemia as well as in chronic ischemia.
- Dilated or hypertrophic cardiomyopathy – Causes 10-15 % of all cases.
- Less common causes (5% of all cases) – Atrial fibrillation with pre-excitation, arrhythmogenic right ventricular cardiomyopathy (ARVC), long QT syndrome (LQTS), Brugada syndrome, aortic stenosis, amyloidosis, third-degree AV-block III without escape rhythm.
Metabolic derangements, electrolyte disorders and exogenous substances, ischemia, etc, may precipitate ventricular arrhythmias in all these patient groups.
Asystole and brady-asystole
As seen in Figure 1, asystole occurs when there is no electrical activity in the heart. The heart is completely still during asystole; i.e. there are no atrial or ventricular depolarizations.
Brady-asystole is defined as asystole interrupted by occasional QRS complexes, but no rhythm capable of producing a noteworthy cardiac output.
Treatment of asystole and brady-asystole
Asystole and brady-asystole are treated according to the resuscitation algorithm.
Pulseless electrical activity (PEA)
Synonym: electromechanical dissociation (EMD)
Pulseless electrical activity is a term applied to any rhythm that is not accompanied by a detectable pulse. It may display complete P, QRS, and T waveforms but no pulse is palpable. This means that the heart’s electrical activity has been dissociated from mechanical contractions, which is why the synonym electromechanical dissociation is often used.
Causes of pulseless electrical activity
The following conditions may cause pulseless electrical activity: hypovolemia, hypoxia, cardiac tamponade, pressure pneumothorax, hypothermia, massive pulmonary embolism, drug overdose, and massive myocardial infarction. The most common of these is myocardial infarction. Massive myocardial infarctions may leave too little viable myocardium to generate stroke volumes that are palpable.
Treatment of pulseless electrical activity
Pulseless electrical activity is treated according to the resuscitation algorithm.

