Clinical ECG Interpretation
-
Introduction to ECG Interpretation6 Chapters
-
Cardiac electrophysiology and ECG interpretation
-
Cardiac electrophysiology: Action potential, automaticity and vectors
-
The ECG leads: Electrodes, limb leads, chest (precordial) leads and the 12-Lead ECG
-
The Cabrera format of the 12-lead ECG and inverted lead aVR
-
ECG interpretation: Characteristics of the normal ECG (P-wave, QRS complex, ST segment, T-wave)
-
How to interpret the ECG: A systematic approach
-
Cardiac electrophysiology and ECG interpretation
-
Arrhythmias and arrhythmology23 Chapters
-
Mechanisms of cardiac arrhythmias: from automaticity to re-entry (reentry)
-
Aberrant ventricular conduction (aberrancy, aberration)
-
Premature ventricular contractions (premature ventricular complex, premature ventricular beats)
-
Premature atrial contraction (premature atrial beat / complex): ECG and clinical implications
-
Sinus rhythm: physiology, ECG criteria & clinical implications
-
Sinus arrhythmia (respiratory sinus arrhythmia)
-
Sinus bradycardia: definitions, ECG, causes and management
-
Chronotropic incompetence (inability to increase heart rate)
-
Sinoatrial arrest & sinoatrial pause (sinus pause / arrest)
-
Sinoatrial block (SA block): ECG criteria, causes and clinical features
-
Sinus node dysfunction (SND) and sick sinus syndrome (SSS)
-
Sinus tachycardia & Inappropriate sinus tachycardia
-
Atrial fibrillation: ECG, classification, causes, risk factors & management
-
Atrial flutter: classification, causes, ECG criteria and management
-
Ectopic atrial rhythm (EAT), atrial tachycardia (AT) & multifocal atrial tachycardia (MAT)
-
Pre-excitation, Atrioventricular Reentrant (Reentry) Tachycardia (AVRT), Wolff-Parkinson-White (WPW) syndrome
-
Junctional rhythm (escape rhythm) and junctional tachycardia
-
Ventricular rhythm and accelerated ventricular rhythm (idioventricular rhythm)
-
Ventricular tachycardia (VT): ECG criteria, causes, classification, treatment
-
Long QT (QTc) interval, long QT syndrome (LQTS) & torsades de pointes
-
Ventricular fibrillation, pulseless electrical activity and sudden cardiac arrest
-
Pacemaker-mediated tachycardia (PMT): ECG and management
-
Diagnosis and management of supraventricular and ventricular tachyarrhythmias: Narrow complex tachycardia & wide complex tachycardia
-
Mechanisms of cardiac arrhythmias: from automaticity to re-entry (reentry)
-
Myocardial Ischemia & Infarction23 Chapters
-
Introduction to Coronary Artery Disease (Ischemic Heart Disease)
-
Classification of Acute Coronary Syndromes (ACS) & Acute Myocardial Infarction (AMI)
-
A New Approach to Acute Coronary Syndromes: Occlusion MI (OMI) vs. non-occlusion MI (NOMI)
-
Clinical application of ECG in chest pain & acute myocardial infarction
-
Diagnostic Criteria for Acute Myocardial Infarction: Cardiac troponins, ECG & Symptoms
-
Cardiac troponin I (TnI) and T (TnT): Interpretation and evaluation in acute coronary syndromes
-
Myocardial Ischemia & infarction: Cellular changes, ECG and symptoms
-
The left ventricle in myocardial ischemia and infarction
-
Factors that modify the natural course in acute myocardial infarction (AMI)
-
ECG in myocardial ischemia: ischemic changes in the ST segment & T-wave
-
ST segment depression in myocardial ischemia and differential diagnoses
-
ST segment elevation in acute myocardial ischemia and differential diagnoses
-
ST elevation myocardial infarction (STEMI) without ST elevations on 12-lead ECG
-
T-waves in ischemia: hyperacute, inverted (negative), Wellen's sign & de Winter's sign
-
ECG signs of myocardial infarction: pathological Q-waves & pathological R-waves
-
Other ECG changes in ischemia and infarction
-
Supraventricular and intraventricular conduction defects in myocardial ischemia and infarction
-
ECG localization of myocardial infarction / ischemia and coronary artery occlusion (culprit)
-
The ECG in assessment of myocardial reperfusion
-
Approach to patients with chest pain: differential diagnoses, management & ECG
-
Stable Coronary Artery Disease (Angina Pectoris): Diagnosis, Evaluation, Management
-
NSTEMI (Non-ST Elevation Myocardial Infarction) & Unstable Angina: Diagnosis, Criteria, ECG, Management
-
STEMI (ST Elevation Myocardial Infarction): Diagnosis, ECG, Criteria, and Management
-
Introduction to Coronary Artery Disease (Ischemic Heart Disease)
-
Conduction Defects11 Chapters
-
Overview of atrioventricular (AV) blocks
-
First-degree AV block (AV block I, AV block 1)
-
Second-degree AV block: Mobitz type 1 (Wenckebach) & Mobitz type 2 block
-
Third-degree AV block (3rd degree AV block, AV block 3, AV block III)
-
Management and treatment of AV block (atrioventricular blocks)
-
Intraventricular conduction delay: bundle branch blocks & fascicular blocks
-
Right bundle branch block (RBBB): ECG, criteria, definitions, causes & treatment
-
Left bundle branch block (LBBB): ECG criteria, causes, management
-
Left bundle branch block (LBBB) in acute myocardial infarction: the Sgarbossa criteria
-
Fascicular block (hemiblock): Left anterior & left posterior fascicular block
-
Nonspecific intraventricular conduction delay (defect)
-
Overview of atrioventricular (AV) blocks
-
Cardiac Hypertrophy & Enlargement5 Chapters
-
Atrial and ventricular enlargement: hypertrophy and dilatation on ECG
-
ECG in left ventricular hypertrophy (LVH): criteria and implications
-
Right ventricular hypertrophy (RVH): ECG criteria & clinical characteristics
-
Biventricular hypertrophy ECG and clinical characteristics
-
Left atrial enlargement (P mitrale) & right atrial enlargement (P pulmonale) on ECG
-
Atrial and ventricular enlargement: hypertrophy and dilatation on ECG
-
Drugs & Electrolyte Imbalance3 Chapters
-
Genetics, Syndromes & Miscellaneous7 Chapters
-
ECG J wave syndromes: hypothermia, early repolarization, hypercalcemia & Brugada syndrome
-
Brugada syndrome: ECG, clinical features and management
-
Early repolarization pattern on ECG (early repolarization syndrome)
-
Takotsubo cardiomyopathy (broken heart syndrome, stress induced cardiomyopathy)
-
Pericarditis, myocarditis & perimyocarditis: ECG, criteria & treatment
-
Eletrical alternans: the ECG in pericardial effusion & cardiac tamponade
-
Long QT Syndrome (LQTS)
-
ECG J wave syndromes: hypothermia, early repolarization, hypercalcemia & Brugada syndrome
-
Exercise Stress Testing (Exercise ECG)6 Chapters
-
Introduction to exercise stress testing (treadmill test, exercise ECG)
-
Indications, Contraindications, and Preparations for Exercise Stress Testing
-
Exercise stress test (exercise ECG): protocols, evaluation & termination
-
Exercise stress testing in special patient populations
-
Exercise physiology: from normal response to myocardial ischemia & chest pain
-
Evaluation of exercise stress test: ECG, symptoms, blood pressure, heart rate, performance
-
Introduction to exercise stress testing (treadmill test, exercise ECG)
Sinoatrial arrest & sinoatrial pause (sinus pause / arrest)
Sinoatrial arrest & sinoatrial pause (sinus pause/arrest): ECG characteristics & clinical implications
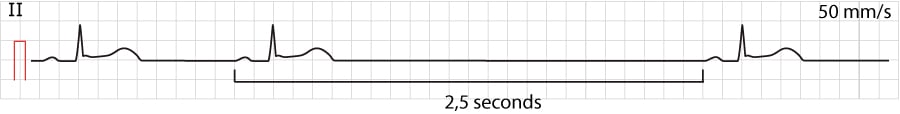
A sinoatrial arrest occurs when the sinoatrial node does not discharge an impulse for ≥2 seconds. Failure to discharge an impulse within <2 seconds is defined as a sinoatrial pause. Refer to Figure 1.
As discussed in Chapter 1, if the sinoatrial node fails to discharge an impulse, three latent pacemaker structures can discharge impulses that will salvage the situation. Latent pacemakers can continue discharging impulses until the sinoatrial node recovers and starts discharging. Less than 3 consecutive beats (or from a latent pacemaker (or any other ectopic focus) are referred to as escape beats. Three or more consecutive beats from a latent pacemaker (or other ectopic focus) are referred to as an escape rhythm.
In most cases, the escape rhythm originates in either of the following three structures (discussed in detail in Chapter 1):
- Specific clusters of atrial myocardium: There are clusters of atrial myocardium that possess automaticity and thus pacemaker function. The intrinsic rate of depolarization in these cells is 60 beats per minute. The resulting P-wave is morphologically different from the sinus P-wave, but the QRS complex is normal (provided that intraventricular conduction is normal). This rhythm may be referred to as atrial rhythm.
- Cells near the atrioventricular node: The atrioventricular node does not possess automaticity, but cells surrounding it do. These cells are capable of generating an escape rhythm with a rate of 40 beats per minute. QRS complexes are normal (provided that intraventricular conduction is normal). If the P-wave is visible, it is retrograde in lead II (because of the reversed direction of atrial activation) and may be located before or after the QRS complex. This rhythm is referred to as a junctional rhythm.
- The His-Purkinje network: All these fibers possess automaticity with an intrinsic rate of depolarization of around 20–40 beats/min. If the impulses are discharged from fibers proximal to the bifurcation of the bundle of His, QRS complexes will be normal (QRS duration <0.12 s), because both bundle branches receive the impulse and spread it. If the impulse is discharged distal to the bifurcation of the bundle of His, the QRS complexes will be wide (QRS duration ≥0.12 s). The escape rhythm with wide QRS complexes is referred to as ventricular rhythm.
All these rhythms are regular. Since there is competition between these latent pacemakers, the one with the fastest intrinsic rate of depolarization will be the pacemaker, which means that it usually is atrial myocardium.
Asystole occurs if no escape rhythm awakes. It is uncommon that sinus arrest leads to persistent asystole; latent pacemakers virtually always awake and salvage the rhythm.
Adam-Stokes attack
Syncope due to sinus arrest is referred to as Adam-Stokes attack.
Causes of sinoatrial arrest/pause
High vagal tone is benign and the most common cause of sinus arrest/pause. It commonly affects younger individuals who endure intense emotional stress, acute pain or other stimuli that increases vagal tone. In all other situations, sinus arrest/pause should be considered abnormal, and the following differential diagnoses are at hand:
- Sinus node dysfunction.
- Side effects of drugs (diltiazem, verapamil, beta-blockers, digitalis).
- Hypoxia.
- Myocardial ischemia/infarction.
- Hyperkalemia.
Treatment of sinoatrial arrest/pause
Sinus arrest/pause due to increased vagal tone does not necessitate treatment but it might be wise to observe the patient for 24 hours (including ECG monitoring). In all other situations, the underlying condition should be targeted and, if necessary, bradycardia should be treated (treatment alternatives are discussed in the article on sinus node dysfunction).
