Introduction to exercise stress testing (treadmill test, exercise ECG)
Introduction to exercise stress test (treadmill test, exercise stress ECG)
- Role of the electrocardiogram (ECG) in exercise stress testing
- Exercise stress testing in the age of non-invasive cardiovascular imaging
- Cardiopulmonary exercise stress test (ergospirometry)
- Safety of exercise stress testing
- Selection of patients
- Pre-test probability: selecting appropriate patients
- Sensitivity and specificity of exercise stress test
- References
Exercise stress testing has been used routinely for over 60 years to evaluate cardiopulmonary function and to diagnose cardiovascular disease. The value of exercise stress testing is evident from the fact that exercise capacity (cardiopulmonary capacity) is one of the strongest predictors of cardiovascular and overall mortality. Thus, the clinical utility of exercise stress testing is immense and the procedure may be used in numerous situations, ranging from health screening to assessment of symptoms after coronary artery bypass surgery. Traditionally, the most common indication for exercise stress testing has been the diagnostic evaluation of coronary artery disease. However, current guidelines (ESC, AHA, ACC) discourage the use of exercise stress testing for the evaluation of coronary artery disease, which is due to the low sensitivity of the method (details below). Sensitivity and specificity are considerably higher for CT angiography, SPECT, echocardiography, and coronary angiography, which are therefore the recommended modalities for the evaluation of coronary artery disease (refer to Evaluation of coronary artery disease and angina pectoris). Yet, exercise stress testing provides a fundamental parameter that cannot be obtained by other imaging methods, namely exercise capacity (and VO2max, see below). In addition to exercise capacity, stress testing also provides information on electrocardiographic (ECG) reaction, the occurrence of arrhythmias, symptoms, physiological reactions (blood pressure, heart rate) during and after exercise, etc.
Exercise stress testing may also be referred to as exercise ECG or exercise tolerance test. Because the vast majority of all exercise stress tests in the United States are performed using a treadmill, the term treadmill test has almost become synonymous with the exercise stress test. However, the term treadmill test should only be used when referring to exercise stress tests carried out on a treadmill. In many parts of the world, the bicycle is preferred over the treadmill, as will be discussed later.
Role of the electrocardiogram (ECG) in exercise stress testing
It is a common misunderstanding that the ECG is the main parameter of the stress test. The ECG reaction is indeed important but several other parameters are equally important. In fact, a large body of evidence demonstrates that the strongest predictor of cardiovascular and overall mortality is maximal (peak) oxygen uptake, which is a measure of cardiovascular fitness and exercise capacity. In clinical practice, however, it is difficult to achieve peak oxygen uptake because it requires maximal exertion, which patients rarely achieve. Patients are usually limited by leg fatigue, discomfort, cardiovascular disease, lack of motivation, etc. Moreover, measuring peak oxygen uptake is technically arduous and therefore peak work intensity is used as a proxy for peak oxygen uptake. This is discussed in detail below.
The purpose of the exercise stress test is to induce cardiovascular stress in order to provoke symptoms, ECG changes, blood pressure response, and heart rate response, as well as assess limiting determinants of exercise capacity. These parameters offer diagnostic and prognostic information which can only be obtained during physical exercise.
Independent of other traditional risk factors, exercise capacity is one of the single best predictors of risk for future adverse events in virtually all patient populations, including apparently healthy individuals.
Exercise stress testing in the age of non-invasive cardiovascular imaging
Advances in computerized tomography (CT), cardiac magnetic resonance imaging (cMRI), and echocardiography have enabled detailed functional and anatomical imaging of cardiac anatomy, assessment of coronary artery stenosis, and myocardial ischemia. These methods offer greater sensitivity and specificity as compared with exercise stress testing. Hence, the exercise stress test is no longer the preferred modality for the evaluation of suspected coronary artery disease. However, exercise stress testing is cheap, widely available, and not dependent on the examiner, it does not confer harmful radiation and provides numerous other parameters that can improve cardiovascular assessment and prognostication. Stress testing also allows for the assessment of the effect of interventions and medications. Furthermore, the exercise stress test provides information on the limiting determinants of exercise capacity (discussed below). The exercise stress test remains one of the most important diagnostic instruments in medicine.
Table 1. Sensitivity and specificity of various modalities to assess coronary artery disease.
| Modality | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Exercise stress testing (exercise ECG) | 40-50% | 85-90% |
| Stress echocardiography | 80-85% | 80-88% |
| Stress SPECT | 73-92% | 63-87% |
| Stress echocardiography with dobutamine | 79-83% | 82-86% |
| Stress MRI with dobutamine | 72-79% | 81-91% |
| Stress echocardiography with vasodilator | 90-91% | 75-84% |
| Stress SPECT with vasodilator | 67-94% | 61-85% |
| CTA coronary artery | 95-99% | 64-83% |
| Stress PET with vasodilator | 91-97% | 74-91% |
Abbreviations: CTA = computed tomography angiography (CT angiography); PET = positron emission tomography; SPECT = single photon emission computed tomography; MR = magnetic resonance. Source: ESC Guidelines (2016).
Purpose of exercise stress testing
Although exercise stress testing is almost synonymous with the assessment of coronary artery disease, the procedure can be used for several other purposes, as follows:
- Assessment of cardiovascular risk.
- Detection of coronary artery disease (ischemic heart disease). Individuals with chest pain (or other symptoms suggestive of myocardial ischemia) can be evaluated using exercise stress testing, although sensitivity is considerably higher with other modalities (Table 1).
- Evaluation of coronary artery disease. Individuals with known ischemic heart disease frequently perform stress tests as part of risk stratification, assessment of functional capacity, limiting determinants, symptoms, and ECG changes. Repeated stress tests are valuable to follow the course of the disease and allow for tailoring patient management.
- Assessment of therapeutic response. Exercise testing can be used to evaluate the effect of medications or interventions such as PCI (percutaneous coronary intervention), CABG (coronary artery bypass grafting), CRT (Cardiac Resynchronization Therapy), etc. The purpose of the exercise test is to evaluate whether such interventions have reduced the intensity or frequency of symptoms or other abnormal signs (e.g. arrhythmias).
- Assessment of perioperative risk for noncardiac surgery: Exercise testing is used routinely to assess perioperative risk indirectly by measuring the cardiovascular response, symptoms, and ECG reaction during exercise.
- Exercise prescription: For some patients, it may be necessary to evaluate functional capacity and exercise response before prescribing exercise. The purpose of the exercise test is to detect significant symptoms and abnormal cardiovascular responses at various levels of intensity. This allows for setting an appropriate level of exercise intensity.
- Determine degree of disability: Exercise stress testing may be used to determine the degree of disability in patients with cardiovascular disease.
Nevertheless, the vast majority of patients referred to exercise stress testing are patients with suspected ischemic heart disease.
Cardiopulmonary exercise stress test (ergospirometry)
Cardiopulmonary exercise testing (CPET, ergospirometry) provides an assessment of the integrative exercise responses involving the pulmonary, musculoskeletal, and cardiovascular systems. This allows for a more comprehensive assessment of these three organ systems. CPET is non-invasive but technically more arduous than traditional exercise stress testing. The use of CPET has increased steadily in the past few decades. The pulmonary measure of main interest is the gas exchange, which is analyzed continuously during the exercise. By analyzing oxygen levels, carbon dioxide levels, respiratory volumes, respiratory frequency, and oxygen uptake, it is possible to estimate cardiac output and peak oxygen uptake, which is the best measure of exercise capacity. Ergospirometry is frequently used for prognostication of heart failure and pulmonary disease.
Safety of exercise stress testing
Exercise testing is a safe procedure. Over six decades of experience and research testify that the risk of complications is very low. It is estimated that approximately 1 death and 2 acute myocardial infarctions are caused per 10,000 tests performed. These estimates vary slightly in different studies, depending on the characteristics of the patient population.
Although exercise testing should not be directly compared with long-distance running, due to differences in the type of workload and the health condition of the participants, it could be interesting to compare the mortality in these two situations. Approximately 1 in 184,000 participants in long-distance races experience a sudden cardiac arrest (JH Kim et al). It follows that the risk is roughly 18 times higher during exercise stress testing. This figure should be viewed in light of the differences in age, risk factors, coexisting conditions, etc, between those performing exercise tests and those performing a marathon.
Indeed, the risk associated with performing an exercise test is very small. The risk that exists is presumably explained by the hazard of provoking myocardial ischemia. Briefly, myocardial ischemia may induce ventricular tachycardia which may degenerate into ventricular fibrillation and cardiac arrest. The risk of ventricular tachycardia depends on the extent of the ischemia (transmural ischemia brings about a great risk of ventricular tachycardia, as compared with subendocardial ischemia which is less hazardous).
Despite the safety of stress testing, patients must be selected with care in order to minimize risk and maximize the usefulness of the procedure.
Selection of patients
The exercise stress test was previously the first choice in patients with suspected ischemic heart disease if the probability of disease was intermediate. The usefulness of the test depends on the patient’s probability of actually having ischemic heart disease. One should therefore begin by assessing the patient’s probability of having ischemic heart disease. This approach is referred to as a Bayesian approach, named after the statistician Thomas Bayes. The Bayesian approach states that the probability that the test will reveal disease depends on the patient’s risk of actually having the disease. This is also referred to as pre-test probability. The pre-test probability depends on risk factors such as age, sex, symptoms, cholesterol levels, smoking status, diabetes status, dietary habits, and so on. Assessing all these variables can be quite cumbersome, which is why the European Society for Cardiology (ESC) suggests are more pragmatic assessment including only age, sex, and symptoms. These three variables are sufficient to estimate a pre-test probability. This will be discussed in detail below.
Thus, pre-test probability is fundamental to assess before referring patients to exercise ECG. It is also important that the patient is capable of performing the test. All patients are not capable of walking on a treadmill, or bicycling, while other patients are not capable of following instructions or communicating verbally. Patients with rheumatic conditions, amputations, severe claudication, etc, may also have difficulties performing the test. These factors must also be taken into consideration.
It is also important to assess whether there are changes in the resting ECG which may impair the evaluation of the ECG reaction during the test.
Changes on the resting ECG which impair the evaluation of the ECG reaction during exercise
The presence of significant ST-T changes on the resting ECG may impair the evaluation of the ECG reaction during exercise. With respect to the ECG, the purpose of the exercise test is to provoke ischemic ECG changes (ST segment depressions). However, there are several conditions that cause ST-T changes (including ST depressions) on the resting ECG and the presence of such will generally make ECG interpretation during exercise more difficult. For example, some conditions may cause ST-T changes which both simulate and mask ischemic ECG changes. The most obvious example is left bundle branch block (LBBB), which causes marked secondary ST-T changes (including ST elevation, ST depression and T-wave inversion) and also masks ischemic ST-T changes. Hence, patients with left bundle branch block on resting ECG should generally not be referred for exercise ECG.
Patients using digoxin (digitalis) may also display significant ST-T changes, particularly ST depressions, on the resting ECG. Such ST depressions are usually generalized, meaning that they are evident in most ECG leads. Digoxin should be withheld 24 hours before exercise testing.
Patients with pre-excitation (Wolff-Parkinson-White syndrome) with delta waves on the resting ECG may not be suitable for exercise ECG. Delta waves are usually associated with secondary ST-T changes which may also impair the ECG interpretation of ischemia.
Patients with pacemakers always display secondary ST-T changes which also renders ischemia detection very difficult. Patients with pacemakers are not suitable for exercise ECG.
Patients with left ventricular hypertrophy (LVH) may display secondary ST-T changes with ST elevations (V1, V2) and ST depressions (V5, V6, aVL, I). The ST depressions may exceed 1 mm on the resting ECG, which renders the exercise test less useful for detecting ischemia. If, however, the ST depressions are less than 1 mm, the exercise test may be useful.
There are also patients with ST segment depressions on the resting ECG without any obvious explanation. As a general rule, if the ST depressions are <1 mm, then the exercise test may be useful.
Note that right bundle branch block (RBBB) does not interfere with the detection of ischemia; i.e. it is fully possible to detect ischemia in the presence of a right bundle branch block. Readers familiar with the appearance of RBBB may know that it is associated with ST depressions (in the J-60 point) in leads V1–V3, but this is rarely a problem since, in the case of myocardial ischemia, ST depressions are rarely confined to V1–V3 because depressions are virtually always seen in V4–V6 as well.
Pre-test probability: selecting appropriate patients
Although exercise stress testing is no longer recommended for the evaluation of coronary artery disease, the rationale for pre-test probability is still relevant to discuss.
As mentioned above, pre-test probability is the likelihood that the patient has coronary artery disease based on symptoms, age and sex. These three variables are strong predictors of coronary artery disease and they are also readily available. The pre-test probability is related to Bayes’ theorem (Thomas Bayes, 1701–1761). This theorem states that the probability of an event is related to circumstances that are associated with the event. In this scenario, the probability of coronary artery disease will be related to age, sex and symptoms. Pre-test probability is easy to assess and it must always be assessed. The purpose of the pre-test probability is as follows:
- Identify patients with a very low probability of disease: these patients most likely do not have the disease and therefore the test is not particularly useful. Furthermore, if they had the disease, it is likely that the disease is very mild and the test will therefore not be able to detect it.
- Identify patients with a very high probability of disease: these patients most likely have the disease and therefore the test will be unnecessary.
Calculation of pre-test probability (PTP)
The likelihood of coronary artery disease is a function of disease prevalence and patient characteristics.
If the patient represents a population with a high prevalence of coronary heart disease and exhibits all symptoms of the disease, then PTP is very high. In that scenario, the usefulness of diagnostic tests decreases because they will almost certainly only confirm an already probable diagnosis. The opposite is also true; if the disease is rare and the patient presents no symptoms consistent with the disease, then an examination is unlikely to reveal anything useful. In general, diagnostic tests are most useful when used in patients with an intermediary likelihood of disease.
- If the probability of coronary heart disease is low and the examination is negative, then coronary heart disease can be excluded.
- If the probability of coronary heart disease is high and the examination is positive, then coronary heart disease can be confirmed.
The pre-test probability of coronary heart disease is estimated based on sex, age, and symptoms (Figure 1).
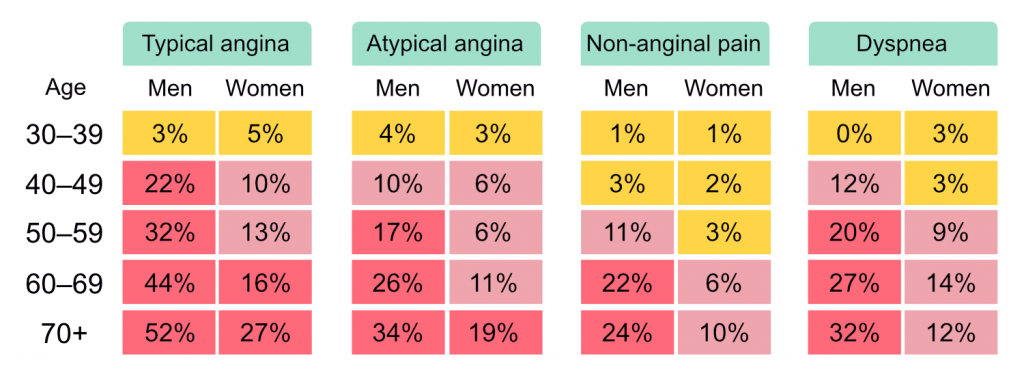
If PTP is <5% then coronary artery disease is unlikely. This should imply that other diagnoses are more likely, and additional investigations for coronary artery disease should only be done in special circumstances. The usefulness of non-invasive tests is greatest if PTP is >15%. If PTP is 5 to 15%, the following parameters should be taken into account for assessing the clinical likelihood of coronary heart disease:
- Risk factors
- Medical history and status
- ECG findings
- Echocardiographic findings.
The clinical probability of coronary artery disease increases with the number of factors that are consistent with coronary artery disease. Thus, the clinical probability of coronary heart disease is the sum of PTP and the above parameters (risk factors, history, status, resting ECG, echocardiography).
Coronary calcium score can be considered when assessing clinical probability. Note, however, that some atherosclerotic plaques have a low calcium concentration, despite high-grade stenosis, which is why calcium score can not be used to exclude coronary heart disease.
Sensitivity and specificity of exercise stress test
Sensitivity and specificity are often used to describe the accuracy of a given diagnostic method. These measures may be defined as follows:
| Sensitivity | The proportion of those with the disease who are detected. |
| Specificity | The proportion of those who are healthy who are correctly classified as such. |
The sensitivity and specificity of exercise stress testing depend on several variables, such as the prevalence of the disease in the population, the criteria used, and so on. The sum of all evidence indicates that sensitivity is around 60–75% and specificity is 60–85% for exercise stress testing. However, sensitivity is lower in people with one-vessel disease (<50% sensitivity) and higher in those with three-vessel or left main stem disease (>85%).
References
Jonathan H Kim, Rajeev Malhotra, George Chiampas, Pierre d’Hemecourt, Chris Troyanos, John Cianca, Rex N Smith, Thomas J Wang, William O Roberts, Paul D Thompson, Aaron L Baggish. Cardiac arrest during long-distance running races. Race Associated Cardiac Arrest Event Registry (RACER) Study Group. N Engl J Med . 2012 Jan 12;366(2):130-40.
