Clinical ECG Interpretation
-
Introduction to ECG Interpretation6 Chapters
-
Cardiac electrophysiology and ECG interpretation
-
Cardiac electrophysiology: Action potential, automaticity and vectors
-
The ECG leads: Electrodes, limb leads, chest (precordial) leads and the 12-Lead ECG
-
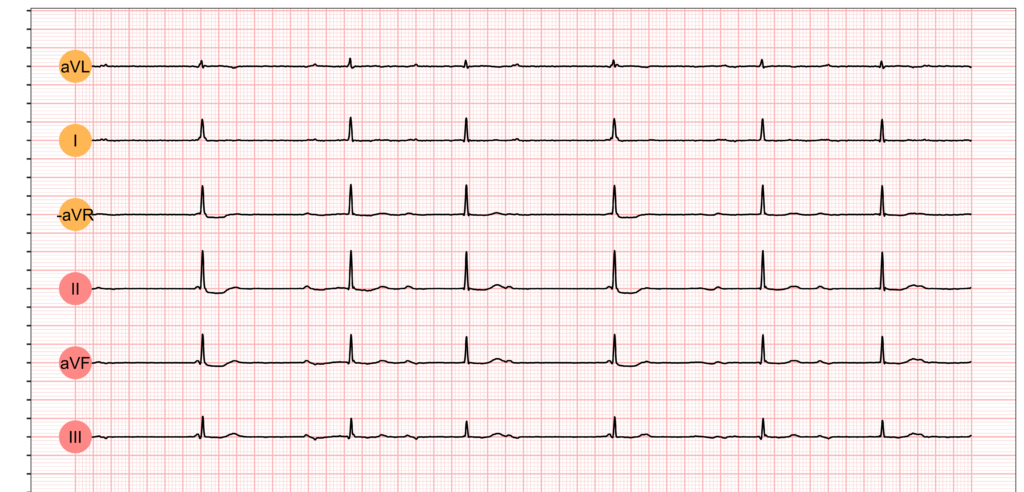
The Cabrera format of the 12-lead ECG & lead –aVR instead of aVR
-
ECG interpretation: Characteristics of the normal ECG (P-wave, QRS complex, ST segment, T-wave)
-
How to interpret the ECG: A systematic approach
-
Cardiac electrophysiology and ECG interpretation
-
Arrhythmias and arrhythmology24 Chapters
-
Mechanisms of cardiac arrhythmias: from automaticity to re-entry (reentry)
-
Aberrant ventricular conduction (aberrancy, aberration)
-
Premature ventricular contractions (premature ventricular complex, premature ventricular beats)
-
Premature atrial contraction (premature atrial beat / complex): ECG & clinical implications
-
Sinus rhythm: physiology, ECG criteria & clinical implications
-
Sinus arrhythmia (respiratory sinus arrhythmia)
-
Sinus bradycardia: definitions, ECG, causes and management
-
Chronotropic incompetence (inability to increase heart rate)
-
Sinoatrial arrest & sinoatrial pause (sinus pause / arrest)
-
Sinoatrial block (SA block): ECG criteria, causes and clinical features
-
Sinus node dysfunction (SND) and sick sinus syndrome (SSS)
-
Sinus tachycardia & Inappropriate sinus tachycardia
-
Atrial fibrillation: ECG, classification, causes, risk factors & management
-
Atrial flutter: classification, causes, ECG diagnosis & management
-
Ectopic atrial rhythm (EAT), atrial tachycardia (AT) & multifocal atrial tachycardia (MAT)
-
Atrioventricular nodal reentry tachycardia (AVNRT): ECG features & management
-
Pre-excitation, Atrioventricular Reentrant (Reentry) Tachycardia (AVRT), Wolff-Parkinson-White (WPW) syndrome
-
Junctional rhythm (escape rhythm) and junctional tachycardia
-
Ventricular rhythm and accelerated ventricular rhythm (idioventricular rhythm)
-
Ventricular tachycardia (VT): ECG criteria, causes, classification, treatment
-
Long QT (QTc) interval, long QT syndrome (LQTS) & torsades de pointes
-
Ventricular fibrillation, pulseless electrical activity and sudden cardiac arrest
-
Pacemaker mediated tachycardia (PMT): ECG and management
-
Diagnosis and management of narrow and wide complex tachycardia
-
Mechanisms of cardiac arrhythmias: from automaticity to re-entry (reentry)
-
Myocardial Ischemia & Infarction22 Chapters
-
Introduction to Coronary Artery Disease (Ischemic Heart Disease) & Use of ECG
-
Classification of Acute Coronary Syndromes (ACS) & Acute Myocardial Infarction (AMI)
-
Clinical application of ECG in chest pain & acute myocardial infarction
-
Diagnostic Criteria for Acute Myocardial Infarction: Cardiac troponins, ECG & Symptoms
-
Cardiac troponin I (TnI) and T (TnT): Interpretation and evaluation in acute coronary syndromes
-
Myocardial Ischemia & infarction: Reactions, ECG Changes & Symptoms
-
The left ventricle in myocardial ischemia and infarction
-
Factors that modify the natural course in acute myocardial infarction (AMI)
-
ECG in myocardial ischemia: ischemic changes in the ST segment & T-wave
-
ST segment depression in myocardial ischemia and differential diagnoses
-
ST segment elevation in acute myocardial ischemia and differential diagnoses
-
ST elevation myocardial infarction (STEMI) without ST elevations on 12-lead ECG
-
T-waves in ischemia: hyperacute, inverted (negative), Wellen's sign & de Winter's sign
-
ECG signs of myocardial infarction: pathological Q-waves & pathological R-waves
-
Other ECG changes in ischemia and infarction
-
Supraventricular and intraventricular conduction defects in myocardial ischemia and infarction
-
ECG localization of myocardial infarction / ischemia and coronary artery occlusion (culprit)
-
The ECG in assessment of myocardial reperfusion
-
Approach to patients with chest pain: differential diagnoses, management & ECG
-
Stable Coronary Artery Disease (Angina Pectoris): Diagnosis, Evaluation, Management
-
NSTEMI (Non ST Elevation Myocardial Infarction) & Unstable Angina: Diagnosis, Criteria, ECG, Management
-
STEMI (ST Elevation Myocardial Infarction): diagnosis, criteria, ECG & management
-
Introduction to Coronary Artery Disease (Ischemic Heart Disease) & Use of ECG
-
Conduction Defects11 Chapters
-
Overview of atrioventricular (AV) blocks
-
First-degree AV block (AV block I, AV block 1)
-
Second-degree AV block: Mobitz type 1 (Wenckebach) & Mobitz type 2 block
-
Third-degree AV block (3rd degree AV block, AV block 3, AV block III)
-
Management and treatment of AV block (atrioventricular blocks)
-
Intraventricular conduction delay: bundle branch blocks & fascicular blocks
-
Right bundle branch block (RBBB): ECG, criteria, definitions, causes & treatment
-
Left bundle branch block (LBBB): ECG criteria, causes, management
-
Left bundle branch block (LBBB) in acute myocardial infarction: the Sgarbossa criteria
-
Fascicular block (hemiblock): Left anterior & left posterior fascicular block
-
Nonspecific intraventricular conduction delay (defect)
-
Overview of atrioventricular (AV) blocks
-
Cardiac Hypertrophy & Enlargement5 Chapters
-
Atrial and ventricular enlargement: hypertrophy and dilatation on ECG
-
ECG in left ventricular hypertrophy (LVH): criteria and implications
-
Right ventricular hypertrophy (RVH): ECG criteria & clinical characteristics
-
Biventricular hypertrophy ECG and clinical characteristics
-
Left atrial enlargement (P mitrale) & right atrial enlargement (P pulmonale) on ECG
-
Atrial and ventricular enlargement: hypertrophy and dilatation on ECG
-
Drugs & Electrolyte Imbalance3 Chapters
-
Genetics, Syndromes & Miscellaneous7 Chapters
-
ECG J wave syndromes: hypothermia, early repolarization, hypercalcemia & Brugada syndrome
-
Brugada syndrome: ECG, clinical features and management
-
Early repolarization pattern on ECG (early repolarization syndrome)
-
Takotsubo cardiomyopathy (broken heart syndrome, stress induced cardiomyopathy)
-
Pericarditis, myocarditis & perimyocarditis: ECG, criteria & treatment
-
Eletrical alternans: the ECG in pericardial effusion & cardiac tamponade
-
Long QT Syndrome (LQTS)
-
ECG J wave syndromes: hypothermia, early repolarization, hypercalcemia & Brugada syndrome
-
Exercise Stress Testing (Exercise ECG)6 Chapters
-
Introduction to exercise stress testing (treadmill test, exercise ECG)
-
Indications, Contraindications, and Preparations for Exercise Stress Testing
-
Exercise stress test (exercise ECG): protocols, evaluation & termination
-
Exercise stress testing in special patient populations
-
Exercise physiology: from normal response to myocardial ischemia & chest pain
-
Evaluation of exercise stress test: ECG, symptoms, blood pressure, heart rate, performance
-
Introduction to exercise stress testing (treadmill test, exercise ECG)
Third-degree AV block (3rd degree AV block, AV block 3, AV block III)
Third-degree (complete) AV block: ECG criteria, clinical characteristics and management
This chapter discusses third-degree AV block, which is synonymous with AV dissociation, complete AV block, AV block III and AV block 3. In third-degree AV block, no atrial impulses are conducted to the ventricles. The atria and the ventricles are electrically dissociated from each other. This condition is referred to as atrioventricular (AV) dissociation. Importantly, for the ventricles to have any electrical (and thus pumping) activity at all, an escape rhythm must arise in an ectopic focus (located distal to the block). Third-degree AV block is a very serious condition because escape rhythms may (1) not occur, (2) occur transiently, or (3) occur but generate insufficient cardiac output. If no escape rhythm occurs, cardiac arrest will ensue.
Chapter content
ToggleProgression from first-degree AV block to third-degree AV block is rare. Progression from second-degree AV block Mobitz type 1 (Wenckebach block) is uncommon. However, second-degree AV block Mobitz type 2 frequently progresses to third-degree AV block.
ECG examples are given in Figure 1.
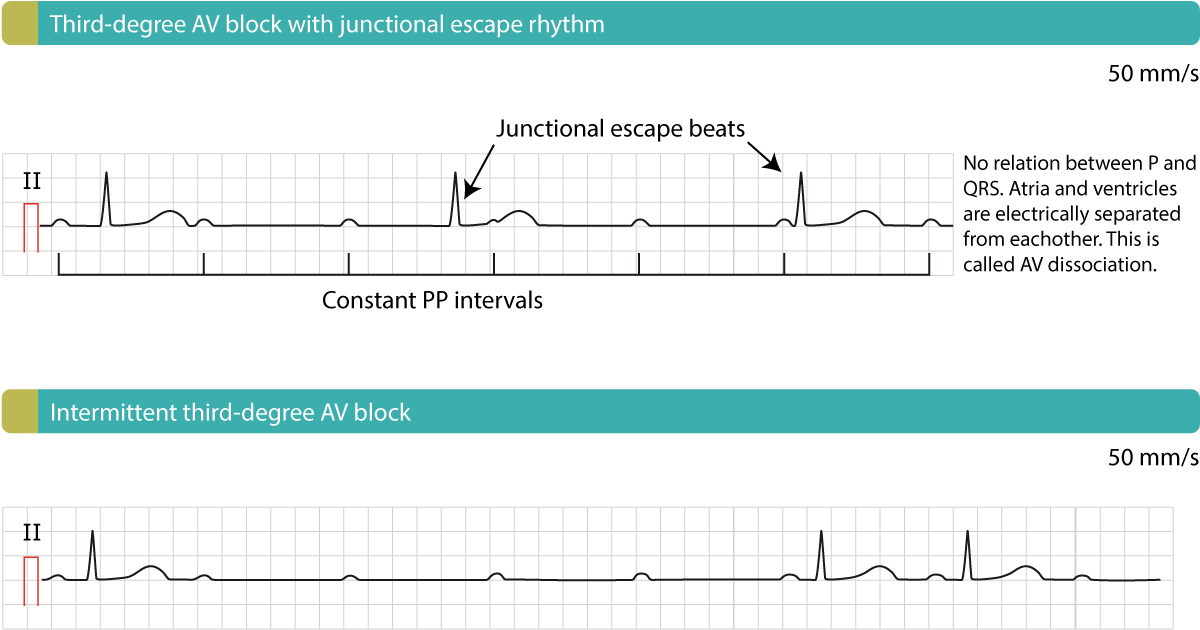
ECG features of third-degree AV block
On the ECG P-waves have no relation to the QRS complexes. The QRS complexes may be normal or wide. P-waves have constant PP interval and ride straight through the strip, without any relation to QRS complexes. P-waves may occur on the ST-T segment (Figure 1, upper panel). The atrial rate is typically faster than the ventricular rate.
It may be very difficult to establish a diagnosis of third-degree AV block if the atrial and ventricular rate is equal and the P-waves occur right before the QRS complexes. This scenario, which is referred to as isoarrhythmic AV block, may even simulate sinus rhythm.
Third-degree AV block causes cardiac arrest unless an escape rhythm emerges. The escape rhythm may have narrow or wide QRS complexes, depending on where the impulses are discharged and whether there is a concomitant bundle branch block. Escape rhythms with narrow QRS complexes indicate that the block and the ectopic focus (which generates the escape rhythm) are located proximal to the bifurcation of the His bundle. This rhythm is often referred to as a junctional escape rhythm. The junctional escape rhythm is regular, with a frequency of roughly 40 beats per minute. If the escape rhythm has wide QRS complexes and a frequency of 20–40 it is most likely a ventricular escape rhythm. Ventricular escape rhythms are unreliable, such that they may cease and thus cause cardiac arrest. Junctional escape rhythm is more reliable (the risk of cardiac arrest is considerably lower). Moreover, ventricular escape rhythms are slow, resulting in reduced cardiac output and risk of hypoperfusion.
Distinguishing AV block 2 and AV block 3
In case the distinction between second-degree AV block and third-degree AV block is difficult, the following rules may be helpful.
- Irregular ventricular rhythm suggests second-degree AV block because escape rhythms in third-degree AV block are regular.
- Regular ventricular rhythm with association between P and QRS and constant PR interval suggests second-degree AV block.
- Regular ventricular rhythm and varying PR interval suggest third-degree AV block because atrial and ventricular rates are most often not equal (which makes the PR interval appear as varying).
Management of third-degree AV block
Please refer to Management of AV block 1, 2 and 3.

