Diagnosis and management of supraventricular and ventricular tachyarrhythmias: Narrow complex tachycardia & wide complex tachycardia
Diagnosis and management of narrow and wide complex tachycardia
- Tachyarrhythmias: causes, differential diagnoses, treatment and management
- Tachycardia: the value of anamnesis
- ECG in tachycardia
- Narrow complex tachycardia (NCT)
- Adenosine for diagnosis and treatment of tachycardia
- Arrhythmia substrates on the resting ECG
- Algorithm for diagnosis and management of narrow complex tachycardia (NCT)
- Wide complex tachycardia (WCT)
All clinically significant supraventricular and ventricular tachyarrhythmias have been reviewed in previous sections. However, given that each arrhythmia has been addressed in isolation, distinguishing between them in clinical scenarios may remain challenging. Effective management of tachycardia requires a comprehensive understanding of differential diagnoses, therapeutic strategies, and evidence-based interventions. Many tachyarrhythmias carry a potential risk of serious morbidity or mortality, underscoring the need for a structured and guideline-directed approach. This chapter focuses on practical diagnostic and therapeutic considerations, with recommendations aligned with current guidelines from both the American Heart Association (AHA) and American College of Cardiology (ACC), as well as the European Society of Cardiology (ESC). The classification of tachyarrhythmias into narrow complex (NCT) and wide complex tachycardia (WCT) will be emphasized, as this distinction significantly informs both diagnostic reasoning and treatment decisions in clinical practice.
Note that the terms tachycardia and tachyarrhythmia will be used interchangeably throughout this chapter. For sake of clarity, however, tachyarrhythmia is defined as an abnormal and rapid heart rate, whereas tachycardia is defined as the subjective perception of a rapid heart rate. These terms are often used interchangeably both in clinical practice and in the literature.
Tachyarrhythmias: causes, differential diagnoses, treatment and management
Any heart rate faster than 100 beats per minute is defined as tachycardia, which is synonymous with tachyarrhythmia. Except for sinus tachycardia during physical activity, all tachycardias should be considered pathological and the task is to clarify the cause of the tachycardia. The cause may range from benign to highly malignant, which is why expeditious management is warranted.
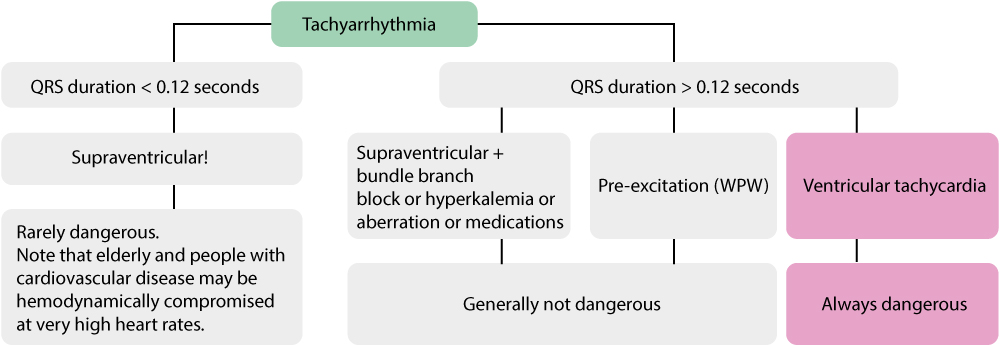
Initial management includes assessing the patient’s clinical status (symptoms, hemodynamics), ECG and risk factors (age, previous disease, medications, laboratory results, etc). Considering the ECG, which is fundamental in all arrhythmias, the first task is to determine whether the arrhythmia is a wide complex tachycardia (WCT) or a narrow complex tachycardia (NCT). This is done by simply judging the QRS duration. If the QRS duration is normal (<0.12 seconds), the arrhythmia is said to be a narrow complex tachycardia (NCT). If the QRS duration is prolonged (≥0.12 seconds), the arrhythmia is a wide complex tachycardia (WCT). This initial distinction will guide the rest of the thinking needed to arrive at a final diagnosis.
The significance of QRS duration in judging arrhythmias can be summarised as follows:
- NCT – Narrow complex tachycardias (QRS duration <0,12 seconds) indicate the ventricles are depolarized via the His-Purkinje system and thus the impulse originates in the atria (i.e the arrhythmia is supraventricular).
- WCT – Wide complex tachycardias (QRS duration ≥0,12 seconds) indicates the ventricles are not depolarized normally. The vast majority of WCTs originate from impulses generated in the ventricles (ventricular tachycardia being the most common arrhythmia). Any impulses generated in the ventricles will result in wide QRS complexes because the impulse will spread entirely or partly outside of the conduction system (which is slow). However, WCTs may be supraventricular, if the tachycardia is accompanied by one of the following conditions: bundle branch block, aberrant ventricular conduction (or simply aberration), hyperkalemia, pre-excitation, certain medications that prolong QRS duration.
Narrow complex tachycardias generally do not cause circulatory compromise and are therefore easier to manage than wide complex tachycardias. The latter (WCT) is in the vast majority of cases caused by ventricular tachycardia (or other ventricular arrhythmias) and may be potentially life-threatening. As always, there are exceptions to these rules. For example, a narrow complex tachycardia may cause circulatory compromise, or even collapse, in an individual with heart failure or ischemic heart disease. For this reason, management of tachycardias actually does not start with judging the ECG, it starts with judging the patient’s symptoms and hemodynamic status. Tachyarrhythmias typically causes one or more of the following symptoms:
- Palpitations
- Dyspnea
- Chest discomfort
- Hypotension
- Syncope/presyncope
- Lightheadedness
- Heart failure
- Renal failure
- Pulmonary edema
- Decreased consciousness
- Shock
- Myocardial infarction
- Cardiac arrest
If the patient displays one or more of the first three symptoms (palpitations, dyspnea, chest discomfort) it is considered safe to take time to judge the ECG and additional information. All other symptoms listed above (highlighted in red) are signs of instability and thus indications for treatment. For clarity, in case of hemodynamic instability (ongoing or impending), the patient must be treated even though a definite diagnosis has not been established. The rationale behind this procedure is simple: treatment with electrical cardioversion is highly effective and terminates most arrhythmias (particularly the life-threatening ones) and early therapy may be life-saving. This is the consensus in North America as well as Europe.
The figure below sums up the discussion so far.
Tachycardia: the value of anamnesis
Anamnesis is as always important. Many tachycardias have a triggering factor, such as physical or emotional stress, coffee consumption, etc. It is always useful to assess whether the tachycardia started abruptly or gradually. This may differentiate several tachycardias. Sinus tachycardia, for example, always starts gradually, whereas AVNRT always starts very abruptly. The patient can determine (as judged by symptoms) the start of the arrhythmia in most cases.
Previous medications, comorbidities and precious ECG tracings should all be assessed. The value of this lies in the fact that if there is any precipitating factor, the arrhythmia is likely to be related to that factor. For example, patients on sotalol medication (which may cause QT prolongation) are likely to have ventricular tachycardia; patients with previous myocardial infarction are very likely to have ventricular tachycardia if they present with a wide complex tachycardia; patients with previous atrial fibrillation are likely to have another episode if they present with an irregular tachycardia and so on.
ECG in tachycardia
The ECG is invaluable in the setting of tachycardia. Although it is often difficult to arrive at a definitive diagnosis, the ECG will allow for a more or less certain diagnosis in most cases. ECG interpretation must, as always, proceed systematically in order to avoid blunders. The following procedure is often used:
- Assess QRS duration to determine whether the tachycardia is a wide complex tachycardia or narrow complex tachycardia.
- Assess ventricular rate and regularity:
- What is the ventricular rate (beats per minute)?
- Is it regular? Is it irregular (but with repeated patterns) or even irregularly irregular (no patterns)?
- Assess electrical axis
- P-waves are extremely important to search for. They are, however, often difficult to spot. If P-waves are invisible, one may try relocating the arm electrodes to various locations on the chest wall. The purpose of this is to simply catch the P-waves and their relation to the QRS complex. Vagus stimulation, adenosine and esophagus ECG may also help reveal the P-waves.
- Are P-waves retrograde in lead II, III and aVF?
- What is the relation, on the ECG, between P-waves and QRS complexes?
- Are P-P intervals regular?
- Is the number of P-waves equal to the number of QRS complexes?
Because the etiology and management of narrow complex tachycardias and wide complex tachycardias differ, these two entities are now discussed separately.
Narrow complex tachycardia (NCT)
Narrow QRS complexes, defined as QRS duration <0.12 seconds, can only be achieved if the ventricles are depolarized via the His-Purkinje system; this allows the impulse to spread rapidly through both ventricles. With very few exceptions, all narrow complex tachycardias (NCT) originate in the atria, hence they are referred to as supraventricular tachycardias. In the vast majority of cases, narrow complex tachycardias do not cause hemodynamic compromise. However, older patients and patients with significant heart disease (particularly with reduced left ventricular function) may develop circulatory compromise. Younger patients and healthy patients generally have no problems enduring tachycardias at rates below 200 beats per minute; higher rates may cause circulatory effects due to reduced stroke volume (shortened diastole means reduced time to fill the ventricles with blood).
Causes of narrow complex tachycardia (NCT)
All differential diagnoses have been discussed in detail in the previous articles. Sinus tachycardia is by far the most common tachycardia. Note that there are no normal causes of sinus tachycardia; there is always a pathological condition (e.g. anemia, heart failure, etc) explaining its existence and that condition must be identified and targeted. Note that sinus tachycardia may be accompanied by frequent premature atrial beats (atrial ectopic beats), which may give the sinus rhythm an irregular ventricular rhythm that may be confused with atrial fibrillation. Also recall inappropriate sinus tachycardia, which is a condition with increased automaticity in the sinoatrial node without any known cause. The last tachycardia arising in the sinoatrial node is sinoatrial nodal reentry tachycardia (SANRT), which is characterized by abrupt onset of sinus tachycardia occurring paroxysmally. It may be difficult, or even impossible, to separate these types of sinus tachycardia. Moreover, atrial tachycardia (also known as ectopic atrial tachycardia) may mimic sinus tachycardia if the P-waves are similar to the sinus P-waves.
Atrioventricular nodal reentry tachycardia (AVNRT), atrioventricular reentry tachycardia (AVRT) and ectopic atrial tachycardia are all caused by reentry (note that 20% of ectopic atrial tachycardias are caused by increased automaticity). These tachycardias arise very abruptly and have a short duration. In most cases, they self-terminate within 30 minutes. All age-groups are at risk of developing these arrhythmias.
Atrial fibrillation and atrial flutter occur in older individuals. Atrial fibrillation must always be the primary suspect if the ECG shows irregular tachycardia without visible P-waves. Atrial flutter is generally regular, characterized by a baseline resembling sawteeth. Atrial flutter may be irregular if there is varying AV-block.
Junctional tachycardia is rare and difficult to discern from AVNRT.
Importantly, all supraventricular tachycardias may display wide QRS complexes if they are accompanied by one of the following conditions/defects:
- Aberrancy (aberration): Aberration (aberrant ventricular conduction) means that a rate-dependent block appears in one of the bundle branches. This typically occurs in the right bundle branch, which has a longer refractory period than the left bundle. It is typical that aberration occurs in the right bundle branch block during rapid acceleration of the heart rate, or if the heart rate is very irregular (refer to Aberrancy / aberrant ventricular conduction).
- Previously existing bundle branch block: Left and right bundle branch block cause wide QRS complexes. Access to earlier ECG tracings (preferably in sinus rhythm) is necessary to verify this.
- Antidromic AVRT: Antidromic AVRT affects individuals with pre-excitation. The re-entry circuit travels from the atria to the ventricles via the accessory pathway and from the ventricles to the atria via the His bundle and atrioventricular node. The QRS complex is wide because ventricular depolarization starts where the accessory pathway inserts in the ventricular myocardium and the impulse spreads from there, entirely or partly outside of the conduction system (which is slow).
- Pacemaker-mediated tachycardia: Pacemakers that stimulate in the ventricle as a response to sensing atrial impulses may cause tachycardia by two mechanisms: (1) an atrial tachyarrhythmia (e.g atrial fibrillation) may be transferred to the ventricles by the pacemaker; (2) the pacemaker impulse may propagate from the ventricles backward to the atria, where the pacemaker electrodes sense the impulse and as a response stimulates again in the ventricles; this cycle repeats itself. Pacemaker beats have wide QRS complexes if the pacemaker stimulates the ventricular myocardium directly (which is very common). Read more in Pacemaker Mediated Tachycardia.
- Hyperkalemia and class I antiarrhythmics: both may prolong the QRS duration. Refer to Beta-blockers and Antiarrhythmic Drugs.
Adenosine for diagnosis and treatment of tachycardia
Adenosine is an endogenous purine nucleoside that modulates many physiological processes in the body. Adenosine acts as a prominent vasodilator in the heart and thus causes increased blood flow in the microcirculation. Adenosine also acts in the atrioventricular node where it slows conduction. The slowing of conduction through the atrioventricular (AV) node is what makes adenosine useful in diagnosing and treating supraventricular tachycardias. Slowing of AV nodal conduction will lead to an increased block of impulses in the AV node and this terminates arrhythmias whose re-entrant pathway involves the AV node. Adenosine will simply render the AV node refractory; when the re-entry impulse encounters the refractory tissue, it is terminated. The arrhythmias are AVNRT and AVRT. Adenosine will also terminate ectopic atrial tachycardias caused by re-entry (which constitutes 80% of atrial tachycardias). Adenosine does not terminate sinus tachycardia, atrial flutter, atrial fibrillation or the remaining ectopic atrial tachycardias. However, in these cases, adenosine will lower the ventricular rate (by increasing the block in the AV node) which may be helpful, as explained below.
Safety of adenosine in the treatment of tachycardia
Adenosine can be administered safely to all individuals with narrow complex tachycardia. It may also be administered, with care, to persons with regular wide complex tachycardias if it is likely that the tachycardia is not a ventricular tachycardia. Adenosine must not be administered during ventricular tachycardia because it may accelerate the ventricular tachycardia and cause hypotension. It is potentially lethal to administer adenosine to patients with irregular wide complex tachycardias because these arrhythmias may be rendered malignant. Irregular wide complex tachycardias may be caused by atrial fibrillation with pre-excitation (i.e atrial fibrillation in a person with accessory pathway). Administration of adenosine may cause AV-block that causes increased impulse conduction over the accessory pathway, by which the atrial fibrillation may propagate to ventricular fibrillation.
Adenosine may induce atrial fibrillation (in up to 12% of patients) and in rare cases even ventricular tachycardia.
To conclude, adenosine can be administered safely to all narrow complex tachycardias. Guidelines recommend the use of adenosine as an initial therapy choice. One should be careful when administering adenosine to regular wide complex tachycardias. Adenosine should never be administered in case of irregular wide complex tachycardias.
Doses and handling of adenosine
Adenosine is injected rapidly in a peripheral venous catheter (6 mg) or central venous catheter (3 mg) followed by flushing with 20 ml saline. The injection may be repeated with a doubled dose (12 mg in peripheral venous catheter, 6 mg in central venous catheter). Heart transplanted individuals are particularly sensitive and should therefore receive only half the dose in a peripheral venous catheter.
Most patients experience chest discomfort during adenosine administration. Anxiety and flushing are also common. Obstructive pulmonary disease is a relative contraindication to adenosine. Theophylline and caffeine reduce sensitivity to adenosine. Heart transplanted patients, and those on dipyramidole, have increased sensitivity. Adenosine dose in the pediatric population is weight-based.
Recall that in case of hemodynamic instability, electrical cardioversion is always the first choice.
Vagal stimulation for diagnosis and treatment of tachycardia
One may always try vagal stimulation before administration of adenosine. Commonly used methods are carotid massage, Valsalva maneuver, and splashing cold water on the face (only done in children). Carotid massage is performed with the patient in the supine position and head rotated slightly away from the side being massaged. The carotid artery is massaged, at the level of the larynx, with two fingers. The massage is best performed with a circulating movement for 10 to 20 seconds. It may be repeated on the opposite side. Correctly performed, this induces a baroreceptor reflex which increases vagal stimulation to the heart and thus increases the block in the AV node. This may terminate 5 to 20% of AVNRT and AVRT.
Vagal stimulation may be used as a diagnostic tool as well. Because of the increased AV nodal block, the ventricular rate is lowered and this may clarify the irregularity of atrial fibrillation; it may demask the characteristics sawtooth-formed baseline in atrial flutter as well. Note that some individuals have very sensitive baroreceptors in the carotid artery and these individuals may be affected by bradycardia or hypotension upon stimulation.
It is extremely rare that atherosclerotic material comes loose and causes stroke during carotid massage. There are, however, some case reports. One should always auscultate the carotid artery before massage and perform it restrictively in persons with known or presumed carotid artery stenosis. In case auscultation reveals murmurs, one should not perform carotid massage.
Analysis of atrial activity (P waves)
Analyzing atrial activity during tachyarrhythmias is crucial but difficult. P-waves may be invisible (hidden in other waveforms) or visible and in the latter case, they may have an abnormal appearance. If the ventricles and the atria are activated simultaneously, the P-wave will be hidden in the QRS complex. If atria and ventricles are not activated simultaneously, but separately, the P-wave may be visible. The direction of the P-wave (positive vs retrograde) depends on the origin of the impulse. If the impulse is discharged near the atrioventricular (AV) node, atrial activation will proceed in the opposite direction and the P-wave will be retrograde in leads normally showing a positive P-wave. If the atrial impulse originates near the sinoatrial (SA) node, the P-wave will appear normal (i.e it will be positive in leads normally showing a positive P-wave).
If P-waves are not clearly visible, one should always compare the ECG waveforms during the tachyarrhythmia with the waveforms durign sinus rhythm (if ECGs are available). Any small waves or deflection that are visible during the tachyarrhythmia, but not during sinus rhythm, may actually represent atrial activity (P-waves). Esophagus ECG, vagal stimulation and adenosine may all facilitate identification of atrial activity.
If no P-waves are visible, the primary suspect is AVNRT. If P-waves are visible, the following must be judged:
- Are P-waves positive or retrograde?
- How fast is the atrial rate?
- Where do P-waves occur, in relation to the QRS complexes?
- Are P-P intervals regular? Completely irregular? Irregular but with a repeating pattern?
- Is the number of P-waves equal to the number of QRS complexes?
At very high atrial rates (>250 atrial beats per minute) one should suspect atrial flutter or atrial tachycardia. Besides this, the atrial rate is of little help.
Positive P-waves in leads II, aVF and III indicate that the impulse originates near the sinoatrial node. If the P-wave during tachycardia is identical to the P-wave during sinus rhythm, the tachycardia originates from the sinoatrial node (differential diagnoses: sinus tachycardia, inappropriate sinus tachycardia, SANRT) or near the sinoatrial node (differential diagnosis: ectopic atrial tachycardia located near the sinoatrial node). If the P-wave is positive but differs morphologically from the sinus P-wave, it is likely to be atrial tachycardia located elsewhere.
Retrograde P-waves are negative in leads II, aVF and III. This indicates that atrial activation is directed oppositely. This suggests AVRT, AVNRT, junctional tachycardia or atrial tachycardia (with ectopic focus near the AV node). Retrograde P-waves are usually associated with short RP intervals (discussed below). Indeed, the RP interval may be so short that the retrograde P-wave is fused with the terminal portion of the QRS complex. The retrograde P-wave will therefore imitate an s-wave in lead II (called “pseudo s”) and an r-wave in V1 (called “pseudo r”). In order to verify pseudo s and pseudo r, one must have a previous ECG recording at hand (and compare the waveforms).
RP interval
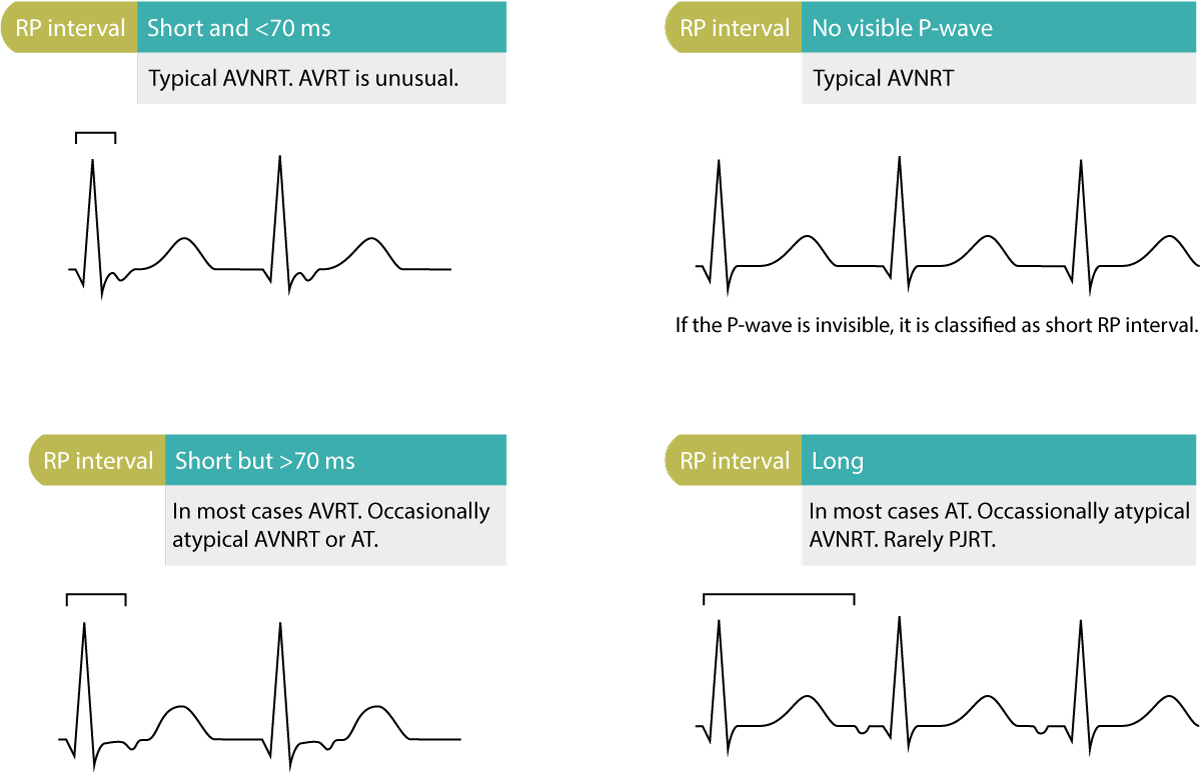
The RP interval must be assessed if there is one P-wave per QRS complex (i.e the ratio of P to QRS is 1:1). The RP interval is the interval from the beginning of the QRS complex to the beginning of the P-wave (Figure 2). The RP interval is either short or long.
A short RP interval is defined as an RP interval being less than half the RR interval (the interval between two R-waves). Short RP interval with retrograde P-wave indicates typical AVNRT or AVRT (rarely ectopic atrial tachycardia located near the AV node). Short RP interval that is <70 milliseconds strongly suggests typical AVNRT. Short RP interval that is >70 ms suggests AVRT. Short RP interval with positive P-wave suggests ectopic atrial tachycardia with first-degree AV-block. Refer to Figure 2.
A long RP interval means that the RP interval is longer than half the RR interval. If the P-wave is retrograde, it is usually ectopic atrial tachycardia with focus near the AV node); it may be atypical AVNRT, orthodromic AVRT with slow accessory pathway (also referred to as PJRT, permanent junctional reciprocating tachycardia). Positive P-waves with long RP interval suggest ectopic atrial tachycardia or sinus tachycardia.
Arrhythmia substrates on the resting ECG
In patients with tachycardia, it is extremely valuable to assess a previous resting ECG (ideally recorded during sinus rhythm). The resting ECG may reveal a wide range of abnormalities that indicate what the etiology of the tachycardia may be. These ECG changes on the resting ECG and their associated arrhythmias are presented in Figure 3.
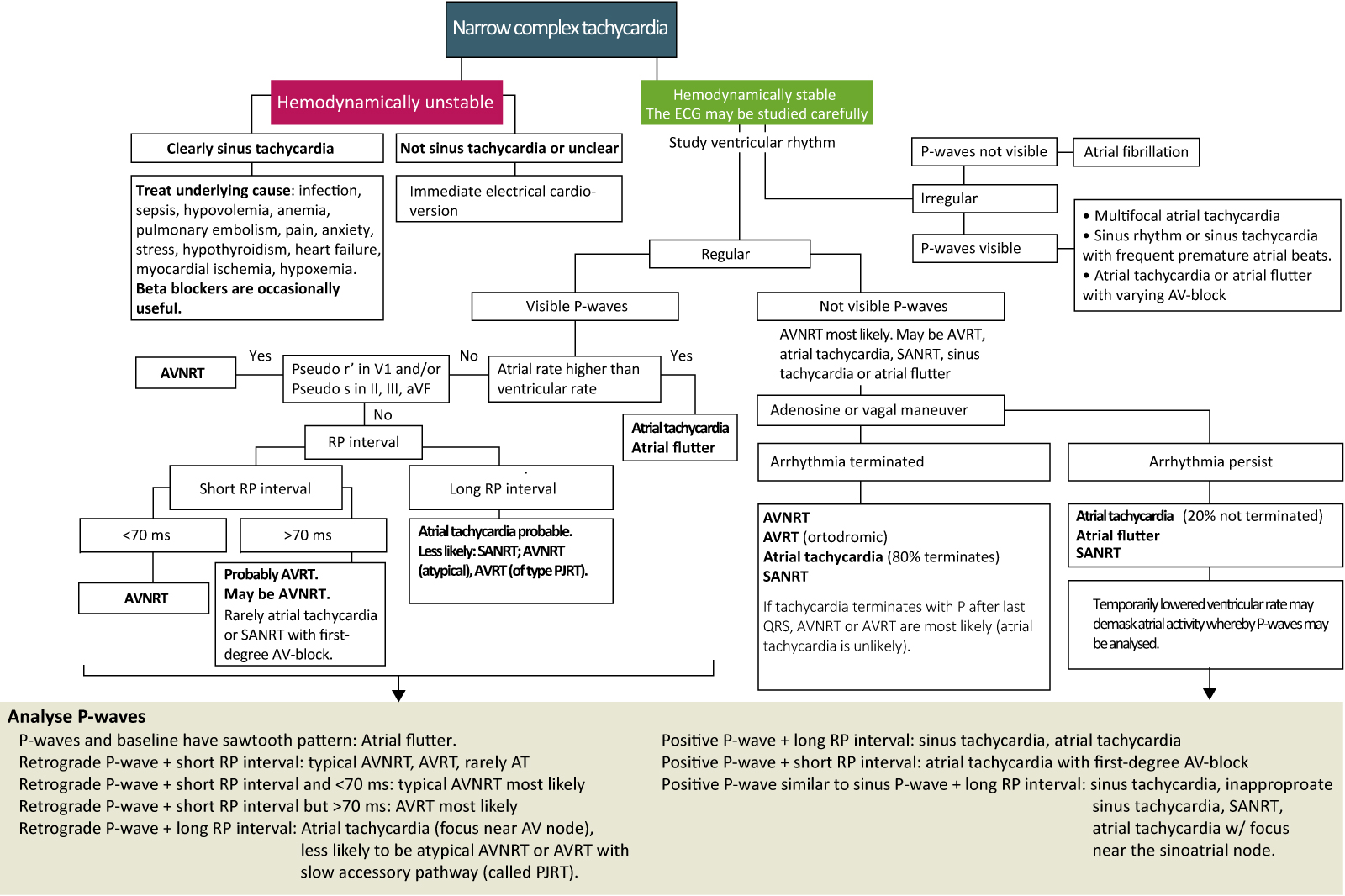
Algorithm for diagnosis and management of narrow complex tachycardia (NCT)
The clinical handling of narrow complex tachycardia is facilitated by using a flow-chart for diagnosis. The flow chart below (Figure 4) is adapted from European and North American guidelines. The corresponding flow chart is later presented for wide complex tachyarrhythmias.
Wide complex tachycardia (WCT)
Tachyarrhythmias with wide (broad) QRS complexes, defined as QRS duration ≥0.12 seconds, are generally more alarming than narrow complex tachycardias. Roughly 80% of all wide complex tachycardias are caused by ventricular tachycardia, and this figure rises to 90% among patients with ischemic heart disease (coronary artery disease). However, approximately 10% of all wide complex tachycardias are actually supraventricular tachycardias accompanied by a factor disturbing ventricular depolarization. Those factors are as follows:
- Existing right bundle branch block or left bundle branch block.
- Aberrant ventricular conduction, i.e bundle branch block occurring due to acceleration of heart rate. (Aberration may occur in other instances, discussed in this article).
- Hyperkalemia
- Class I antiarrhythmic drugs.
- Pacemaker-induced tachycardia.
- Antidromic AVRT.
Nevertheless, the majority of wide complex tachycardias are ventricular tachycardias, which also means that the majority of patients presenting with wide complex tachycardias are at risk of developing unstable hemodynamics and even more malignant arrhythmias (ventricular fibrillation and asystole).
It is crucial to compare the ECG during tachycardia with the ECG during sinus rhythm if such is available. If earlier ECG reveals intraventricular conduction defects (left bundle branch block, right bundle branch block, or any other unspecified conduction defect that prolongs the QRS duration), one must compare the waveforms with those seen during tachycardia. IF the waveforms (QRS-ST-T) are similar during sinus rhythm and tachycardia, it is likely that the tachycardia is supraventricular in origin.
Pacemaker-mediated tachycardia must always be suspected in patients with artificial pacemakers. The pacemaker spike (stimulation artifact) reveals the pacemaker. Modern pacemakers (bipolar pacemakers) may produce a very minute pacemaker spike. In case the pacemaker spikes are not clearly visible, the following suggest pacemaker mediated tachycardia:
- Left bundle branch block pattern (pacemaker stimulate in the right ventricle, which yields QRS with left bundle branch block pattern)
- Wide R-wave in lead I.
Supraventricular tachycardias with wide QRS due to hyperkalemia are uncommon and easy to diagnose with blood analyze of potassium levels.
Aberrant ventricular conduction is fairly common and may be difficult to distinguish from ventricular tachycardia. The same is true for antidromic AVRT, which actually may be impossible to differentiate from ventricular tachycardia. However, antidromic AVRT constitutes <5% of all wide complex tachycardias.
Initial management of wide complex tachycardias (WCT)
Hemodynamic status must be assessed immediately because it may be unstable. If there are signs of compromised hemodynamics (hypotension, angina, chest discomfort, heart failure, lightheadedness etc) the patient should be treated with synchronized electrical cardioversion, even before a diagnosis has been established. A wide complex tachycardia is considered as a ventricular tachycardia until proven otherwise, and in the case of affected circulation it is highly likely that the arrhythmia is ventricular tachycardia. Note that some patients with ventricular tachycardia may be hemodynamically stable initially; sustained ventricular tachycardias, however, always cause circulatory symptoms. The greater the cardiac function, the less pronounced the symptoms.
Unconscious and pulselss patients are managed with advanced cardiac life support.
If the patient is hemodynamically stable, one may study the ECG carefully and attempt treating the arrhythmia pharmacologically. Pharmacological treatment alternatives have been discussed previously. A flow-chart with treatment and management is presented in Figure 5.
Characteristics of patients with wide complex tachycardia (WCT)
Medical history and use of medications must be assessed. Older age and the presence of structural heart disease increase the probability of ventricular tachycardia. Individuals presenting with wide complex tachycardia after recent myocardial infarction virtually always have ventricular tachycardia. All medications are of interest, including medications that prolong the QT interval, because this predisposes for polymorphic ventricular tachycardia. Class I antiarrhythmics may cause both aberrant conduction and ventricular tachycardia. Digoxin may also cause ventricular tachycardia (of all types), but it may also cause all supraventricular tachycardias. Digoxin is particularly arrhythmogenic during hypokalemia. Diuretics predispose to ventricular tachycardia due to side effects (hypokalemia, hypomagnesemia); torsade de pointes is not too uncommon.
Diagnostic maneuvers in wide complex tachycardia (WCT)
Vagal stimulation rarely terminates ventricular tachycardia. It may, however, increase blocking in the AV node, which may (if the arrhythmia is supraventricular) increase RR intervals and reveal AV dissociation. Verapamil, adenosine and beta-blockers are all hazardous in case of ventricular tachycardia (risk of developing hypotension and cardiac arrest). These drugs may be used if one is certain that the wide complex tachycardia is a supraventricular arrhythmia. If the arrhythmia is terminated by adenosine, digoxin, verapamil or diltiazem, one can be virtually certain that it had a supraventricular origin. Termination by means of lidocaine suggests ventricular tachycardia, although AVRT may also be terminated by lidocaine. Termination by means of procainamide or amiodarone does not differentiate ventricular from supraventricular origin.
The following algorithm, which should be at hand always, presents diagnosis and management of wide complex tachycardia.

