Clinical ECG Interpretation
-
Introduction to ECG Interpretation6 Chapters
-
Cardiac electrophysiology and ECG interpretation
-
Cardiac electrophysiology: Action potential, automaticity and vectors
-
The ECG leads: Electrodes, limb leads, chest (precordial) leads and the 12-Lead ECG
-
The Cabrera format of the 12-lead ECG & lead –aVR instead of aVR
-
ECG interpretation: Characteristics of the normal ECG (P-wave, QRS complex, ST segment, T-wave)
-
How to interpret the ECG: A systematic approach
-
Cardiac electrophysiology and ECG interpretation
-
Arrhythmias and arrhythmology24 Chapters
-
Mechanisms of cardiac arrhythmias: from automaticity to re-entry (reentry)
-
Aberrant ventricular conduction (aberrancy, aberration)
-
Premature ventricular contractions (premature ventricular complex, premature ventricular beats)
-
Premature atrial contraction (premature atrial beat / complex): ECG & clinical implications
-
Sinus rhythm: physiology, ECG criteria & clinical implications
-
Sinus arrhythmia (respiratory sinus arrhythmia)
-
Sinus bradycardia: definitions, ECG, causes and management
-
Chronotropic incompetence (inability to increase heart rate)
-
Sinoatrial arrest & sinoatrial pause (sinus pause / arrest)
-
Sinoatrial block (SA block): ECG criteria, causes and clinical features
-
Sinus node dysfunction (SND) and sick sinus syndrome (SSS)
-
Sinus tachycardia & Inappropriate sinus tachycardia
-
Atrial fibrillation: ECG, classification, causes, risk factors & management
-
Atrial flutter: classification, causes, ECG diagnosis & management
-
Ectopic atrial rhythm (EAT), atrial tachycardia (AT) & multifocal atrial tachycardia (MAT)
-
Atrioventricular nodal reentry tachycardia (AVNRT): ECG features & management
-
Pre-excitation, Atrioventricular Reentrant (Reentry) Tachycardia (AVRT), Wolff-Parkinson-White (WPW) syndrome
-
Junctional rhythm (escape rhythm) and junctional tachycardia
-
Ventricular rhythm and accelerated ventricular rhythm (idioventricular rhythm)
-
Ventricular tachycardia (VT): ECG criteria, causes, classification, treatment
-
Long QT (QTc) interval, long QT syndrome (LQTS) & torsades de pointes
-
Ventricular fibrillation, pulseless electrical activity and sudden cardiac arrest
-
Pacemaker mediated tachycardia (PMT): ECG and management
-
Diagnosis and management of narrow and wide complex tachycardia
-
Mechanisms of cardiac arrhythmias: from automaticity to re-entry (reentry)
-
Myocardial Ischemia & Infarction22 Chapters
-
Introduction to Coronary Artery Disease (Ischemic Heart Disease) & Use of ECG
-
Classification of Acute Coronary Syndromes (ACS) & Acute Myocardial Infarction (AMI)
-
Clinical application of ECG in chest pain & acute myocardial infarction
-
Diagnostic Criteria for Acute Myocardial Infarction: Cardiac troponins, ECG & Symptoms
-
Cardiac troponin I (TnI) and T (TnT): Interpretation and evaluation in acute coronary syndromes
-
Myocardial Ischemia & infarction: Reactions, ECG Changes & Symptoms
-
The left ventricle in myocardial ischemia and infarction
-
Factors that modify the natural course in acute myocardial infarction (AMI)
-
ECG in myocardial ischemia: ischemic changes in the ST segment & T-wave
-
ST segment depression in myocardial ischemia and differential diagnoses
-
ST segment elevation in acute myocardial ischemia and differential diagnoses
-
ST elevation myocardial infarction (STEMI) without ST elevations on 12-lead ECG
-
T-waves in ischemia: hyperacute, inverted (negative), Wellen's sign & de Winter's sign
-
ECG signs of myocardial infarction: pathological Q-waves & pathological R-waves
-
Other ECG changes in ischemia and infarction
-
Supraventricular and intraventricular conduction defects in myocardial ischemia and infarction
-
ECG localization of myocardial infarction / ischemia and coronary artery occlusion (culprit)
-
The ECG in assessment of myocardial reperfusion
-
Approach to patients with chest pain: differential diagnoses, management & ECG
-
Stable Coronary Artery Disease (Angina Pectoris): Diagnosis, Evaluation, Management
-
NSTEMI (Non ST Elevation Myocardial Infarction) & Unstable Angina: Diagnosis, Criteria, ECG, Management
-
STEMI (ST Elevation Myocardial Infarction): diagnosis, criteria, ECG & management
-
Introduction to Coronary Artery Disease (Ischemic Heart Disease) & Use of ECG
-
Conduction Defects11 Chapters
-
Overview of atrioventricular (AV) blocks
-
First-degree AV block (AV block I, AV block 1)
-
Second-degree AV block: Mobitz type 1 (Wenckebach) & Mobitz type 2 block
-
Third-degree AV block (3rd degree AV block, AV block 3, AV block III)
-
Management and treatment of AV block (atrioventricular blocks)
-
Intraventricular conduction delay: bundle branch blocks & fascicular blocks
-
Right bundle branch block (RBBB): ECG, criteria, definitions, causes & treatment
-
Left bundle branch block (LBBB): ECG criteria, causes, management
-
Left bundle branch block (LBBB) in acute myocardial infarction: the Sgarbossa criteria
-
Fascicular block (hemiblock): Left anterior & left posterior fascicular block
-
Nonspecific intraventricular conduction delay (defect)
-
Overview of atrioventricular (AV) blocks
-
Cardiac Hypertrophy & Enlargement5 Chapters
-
Atrial and ventricular enlargement: hypertrophy and dilatation on ECG
-
ECG in left ventricular hypertrophy (LVH): criteria and implications
-
Right ventricular hypertrophy (RVH): ECG criteria & clinical characteristics
-
Biventricular hypertrophy ECG and clinical characteristics
-
Left atrial enlargement (P mitrale) & right atrial enlargement (P pulmonale) on ECG
-
Atrial and ventricular enlargement: hypertrophy and dilatation on ECG
-
Drugs & Electrolyte Imbalance3 Chapters
-
Genetics, Syndromes & Miscellaneous7 Chapters
-
ECG J wave syndromes: hypothermia, early repolarization, hypercalcemia & Brugada syndrome
-
Brugada syndrome: ECG, clinical features and management
-
Early repolarization pattern on ECG (early repolarization syndrome)
-
Takotsubo cardiomyopathy (broken heart syndrome, stress induced cardiomyopathy)
-
Pericarditis, myocarditis & perimyocarditis: ECG, criteria & treatment
-
Eletrical alternans: the ECG in pericardial effusion & cardiac tamponade
-
Long QT Syndrome (LQTS)
-
ECG J wave syndromes: hypothermia, early repolarization, hypercalcemia & Brugada syndrome
-
Exercise Stress Testing (Exercise ECG)6 Chapters
-
Introduction to exercise stress testing (treadmill test, exercise ECG)
-
Indications, Contraindications, and Preparations for Exercise Stress Testing
-
Exercise stress test (exercise ECG): protocols, evaluation & termination
-
Exercise stress testing in special patient populations
-
Exercise physiology: from normal response to myocardial ischemia & chest pain
-
Evaluation of exercise stress test: ECG, symptoms, blood pressure, heart rate, performance
-
Introduction to exercise stress testing (treadmill test, exercise ECG)
The ECG in assessment of myocardial reperfusion
The ECG in assessment of myocardial reperfusion
The ECG is an invaluable tool to assess whether an occlusion has been resolved and blood flow has been restored. This assessment is performed daily in the catheterization laboratory in patients undergoing acute PCI. The PCI operator may use the ECG in order to obtain immediate confirmation on whether the intervention was successful. This is particularly important in STE-ACS (STEMI) and the following parameters on the ECG are assessed:
Chapter content
Toggle- Normalization (return) of ST-segment elevations
- Rapid T-wave inversion
Normalization (return) of ST-segment elevations
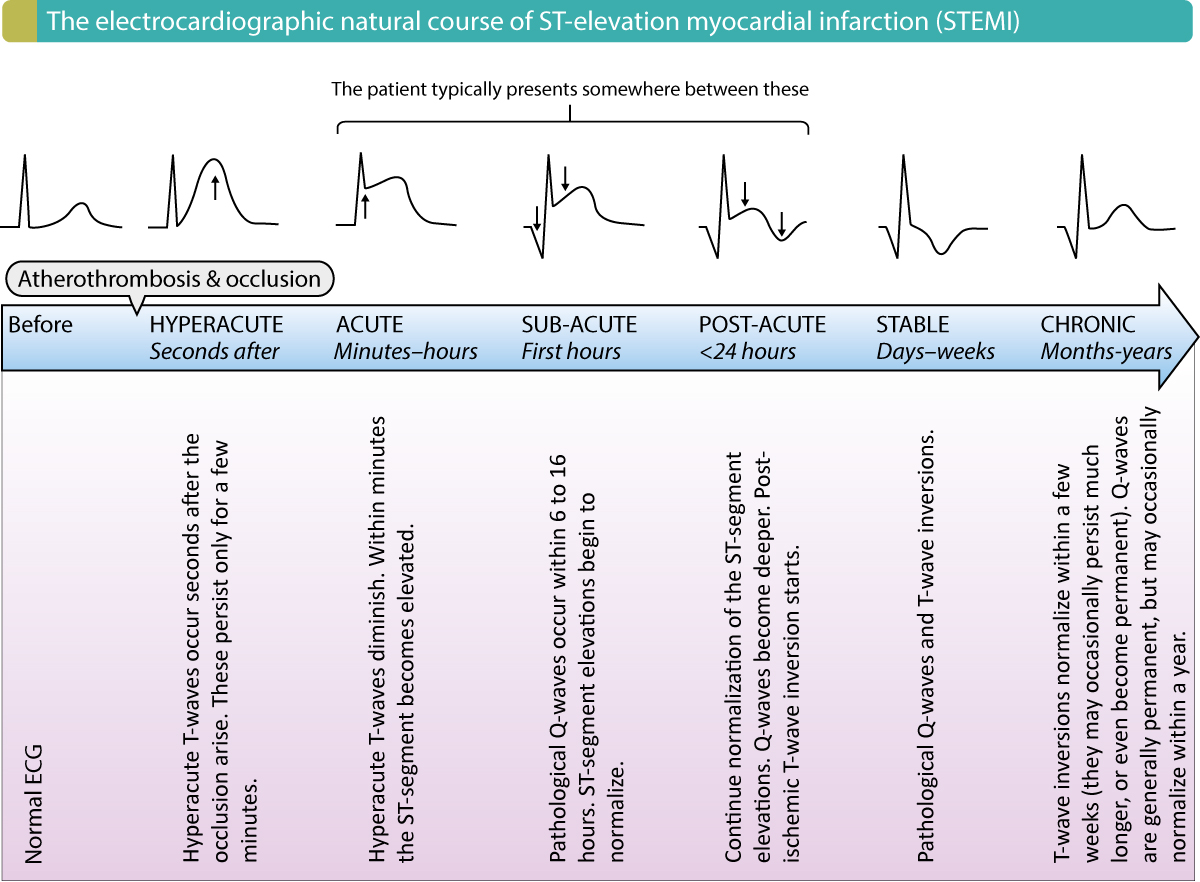
Successful reperfusion results in rapid and marked normalization (return) of ST-segment elevations. If the reperfusion is complete (after a total occlusion) the ST-segment is normalized within one hour, and this confirms that the coronary artery flow is patent. The rapid ST-segment return is explained by rapid normalization of myocardial cell membrane potentials in the ischemic area. Myocardial cells are capable of normalizing their membrane potentials immediately as oxygen becomes available. Recall that ST-segment elevations also become normalized as a part of the natural course of myocardial infarction (refer to Figure 2 below). However, that type of normalization is much slower and it is explained by the gradual death (and thus the disappearance of membrane potential) in the ischemic area.
ECG is a better marker of reperfusion than angiography itself. Studies have shown that angiographic blood flow does not always correlate with myocardial perfusion on the microvascular level. This presumably explained by distal microembolization and dysfunctional microcirculation. Indeed, studies show that 15–35% of patients with STE-ACS/STEMI have inadequate microvascular flow despite patent epicardial blood flow. In such cases, the ECG will be more sensitive (and show a lesser amount of normalization) than evident from angiography. Thus, the ECG is the preferred method of quantifying microvascular blood flow in the myocardium, simply because ST-T changes directly reflect myocardial perfusion.
ST-segment return is particularly important to assess in patients treated with thrombolysis, because reperfusion may be inadequate and/or transient with thrombolysis therapy (PCI is superior to thrombolysis also in this aspect). Guidelines recommend that thrombolysis should result in 50% ST-segment return (i.e reduction of the ST-segment elevation by 50%) within 60 minutes after administration of thrombolysis. Otherwise, one must consider rescue-PCI.
For the purpose of assessing ST-segment return, one should preferably use continuous ST-segment monitoring. If monitoring equipment is not available, 12-lead ECGs should be repeated every 5–10 minutes, while observing the patient’s symptoms. ST-segment return is quantified in the leads with the highest ST-segment elevation.
Inversion of T-waves indicate reperfusion
The slow natural normalization of ST-segment elevation (in untreated patients) is depicted in Figure 2. As evident, such ST-segment elevations are succeeded by gradual inversion of the T-waves. These T-waves are called post-ischemic T-waves and they indicate that the infarction process is more or less completed. Post-ischemic T-wave inversions emerge at the earliest 4–6 hours after an episode of ischemia/infarction, but no later than 24 hours. However, T-wave inversions following reperfusion develop within 4 hours and such T-waves are robust indicators of successful reperfusion (patent artery). This is also associated with better prognosis, return of R-wave amplitudes, and improved left ventricular function.
Accelerated ventricular rhythm (idioventricular rhythm)
This rhythm has been discussed previously in this article. Briefly, accelerated ventricular rhythm (also called idioventricular rhythm) is a benign ventricular rhythm with a heart rate of 60–100 beats per minute (faster than ventricular rhythm, but slower than ventricular tachycardia). Idioventricular rhythm is seen in 15–50% of patients undergoing reperfusion and it indicates that reperfusion has been successful and the artery is patent. This arrhythmia rarely causes hemodynamic effects and terminates spontaneously after a few minutes. No studies have found an association between this rhythm and survival.

