Cardiac troponin I (TnI) and T (TnT): Interpretation and evaluation in acute coronary syndromes
Troponin is a protein complex expressed in cardiac and skeletal muscle. The complex consists of troponin I (TnI), troponin C (TnC) and troponin T (TnT), which enable the interaction between actin and myosin and are therefore fundamental to muscle contraction. There are cardiac-specific isoforms of troponin and these are abbreviated cTnI, cTnT, and cTnC. The isoforms cTnI and cTnT are specific to cardiac muscle cells. Cardiac troponin levels are extremely low in healthy subjects; the 99th percentile is less than a few nanograms per liter of blood (typically <5 ng/L). This is explained by the low turnover of cardiac muscle cells (Parmacek et al). Cardiac troponin levels rise within a few hours after the onset of myocardial infarction. This is utilized in clinical practice by detecting troponins in patients with suspected acute coronary syndromes. Several manufacturers have developed highly sensitive troponin assays for troponin I (cTnI) and troponin T (cTNT). The following differences exist between troponin I and T:
- An increase in troponin I (cTnI) is only seen in myocardial injury. Hence, cTnI is the most cardiac-specific biomarker. Troponin T (cTnT) is cardiac specific but the cTnT assays also detect proteins released from skeletal muscle. Consequently, skeletal muscle damage or inflammation may result in elevated cTnT levels.
- Although both troponin T and I may be chronically elevated in patients with renal failure, this is more pronounced for troponin T (Seng et al).
- Troponin I rises faster than troponin T in acute myocardial infarction.
- Troponin I levels are substantially higher than troponin T levels in acute myocardial infarction. Troponin I levels may be up to 100 times higher than troponin T in the same individual. Hence, higher troponin levels should be expected when converting from troponin T to troponin I assays. No conversion formula (between troponin I and T) has been validated.
- The risk of interference with antibodies in the blood is higher for troponin I (cTnI). Antibody interference is a rare phenomenon that occurs when troponin forms complexes with immunoglobulins, leading to higher levels of troponin being detected with conventional assays. False positive elevations of troponin are rarely explained by such interference (Bularga et al).
Age, sex and renal function affect baseline troponin levels. Troponin levels are up to 3-fold higher in healthy elderly compared with healthy young individuals. Similarly, subjects with severely reduced glomerular filtration rate (GFR) have up to 3-fold higher troponin levels, as compared with individuals with normal GFR. Men have approximately twice as high troponin, as compared with women (Mueller et al, Boeddinghaus et al, Miller-Hodges et al, Twerenbold et al)
Kinetics
- Troponin T (cTnT) and troponin I (cTnI) increase 2-3 hours after the onset of acute myocardial infarction.
- The maximum troponin value is observed in 12–48 hours.
- Troponin may be elevated for up to 2 weeks after a heart attack.
- The larger the infarction, the higher the troponin level and the longer the duration of elevated troponin levels.
Differences in absolute concentrations of troponin I and T during acute myocardial infarction
As noted above, cardiac troponin I (cTnI) concentrations tend to increase to higher levels than cTnT during acute myocardial infarction. cTnI and cTnT have different molecular structures, which may affect their release into the blood as well as their clearance. cTnI has a smaller molecular weight (35 kDa) than cTnT (37 kDa), and a faster release kinetics. This may explain higher peak levels of cTnI compared with cTnT.
Normal values (reference values)
- URL (upper reference limit): The URL is the upper normal limit of troponin in a normal (healthy) population. It is defined as the 99th percentile in healthy subjects. The 99th percentile varies among different assays (see Table 1), with values between 10 ng/L and 20 ng/L being most common.
- Elevated troponin: A value above the URL (99th percentile) is considered elevated.
The type of assay and algorithm used to rule out or rule in acute myocardial infarction varies across regions and nations. Currently, the 0h / 1h and 0h / 2h algorithms are the most widely used algorithms (discussed below).
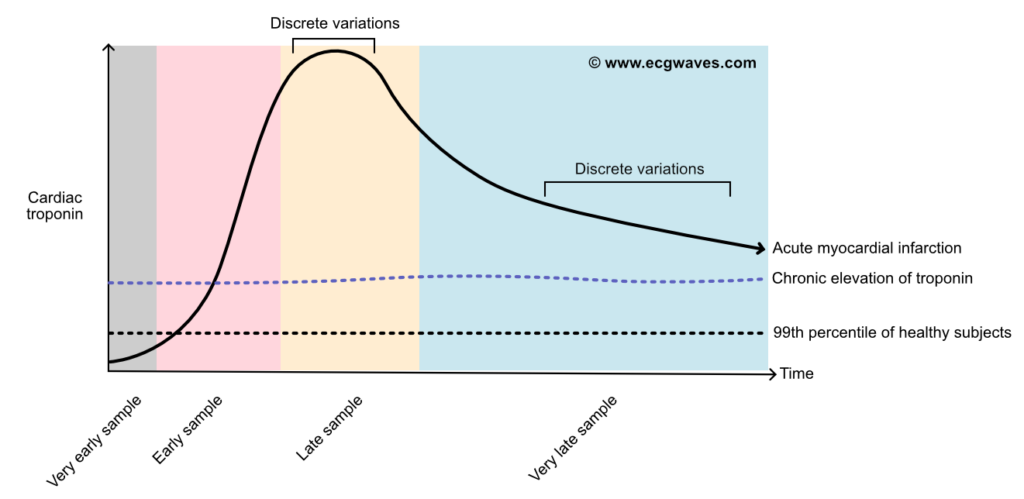
Fundamental to the diagnosis of acute myocardial infarction is the confirmation of rising and/or falling troponin levels. The changing (i.e rising or falling) levels differentiate acute myocardial infarction from chronic elevations (e.g due to heart failure, renal failure, etc).
High-sensitivity troponin (hs-troponin)
High-sensitivity troponin (hs-troponin) assays have been adopted in most hospitals. The definition of high-sensitivity assays is that it is able to detect troponin in healthy subjects without myocardial injury (i.e a few nanograms of troponin per liter blood). Thus, high-sensitivity troponin assays can detect troponin in healthy individuals. Values above the 99th percentile for healthy subjects are considered abnormal.
High-sensitivity troponin is approximately 1000 times more sensitive than the previous generation of troponin assays. The introduction of high-sensitivity troponin, therefore, resulted in a substantial proportion (approximately 20%) of patients with unstable angina being re-classified as NSTEMI (Braunwald et al, Collet et al, Mueller et al).
High-sensitivity troponins have several advantages over previous assays, namely:
- Hs-troponin assays detect troponin elevations earlier than previous assays.
- The negative predictive value (NPV) for hs-troponin is higher than in previous assays.
- A substantial proportion (~20%) of cases previously classified as unstable angina can be correctly classified as NSTEMI.
- The positive predictive value (PPV) for troponin levels elevated 5-fold the URL is 90% for type 1 myocardial infarction.
Troponin in acute myocardial infarction
A diagnosis of acute myocardial infarction is made when troponin levels are elevated (with rising or falling levels) and the patient exhibits at least one of the following:
- ECG changes consistent with myocardial ischemia.
- Imaging evidence of myocardial infarction (CMR, SPECT, echocardiography).
- Symptoms consistent with myocardial infarction.
Interpretation of elevated troponin levels
- Myocardial injury (infarction) requires at least one troponin value above the 99th percentile.
- In acute myocardial injury (including infarction) the troponin level should rise or fall during repeated sampling.
- To rule in or rule out acute myocardial infarction ≥2 analyses of troponin are obtained. The following algorithms exist (discussed below):
- The 0 h / 1 h algorithm: Troponin is analyzed immediately on arrival (0 h) and after 1 hour.
- The 0 h / 2 h algorithm: Troponin is analyzed immediately on arrival (0 h) and after 2 hours.
- The 0 h / 3 h algorithm: Troponin is analyzed immediately on arrival (0 h) and after 3 hours.
- In chronic myocardial injury the troponin elevation is typically persistent, without significant dynamics during repeated sampling.
Pitfalls, caveats and confounders in interpreting troponin levels
- Patients with unstable angina pectoris do not have elevated troponin levels. Unstable angina is an acute coronary syndrome (ACS).
- In the late course and very late course of myocardial infarction (Figure 1), troponin levels may remain relatively unchanged between two measurements (taken at short intervals), thus not allowing for the detection of a clear rise or fall in troponin.
- The 0 h / 1 h and 0 h / 2 h algorithms apply to all patients in the emergency room, regardless of chest pain onset. However, only a minority of patients in the validation studies presented within 1 hour, which causes some uncertainty in patients presenting very early. Additional measurements of troponin should be considered in patients presenting very early (<1 h after chest pain onset).
- In less than 1% of cases of myocardial infarction, troponin release is slower than normal, causing a delay in troponin elevation. If suspicion of myocardial infarction remains high, additional troponin measurements should be considered.
Causes of elevated troponin levels
A long range of conditions can lead to elevated cardiac troponin levels. The magnitude or course of the elevation does not clarify the cause of the injury. The most likely cause of the troponin elevation is indicated by the clinical context. Below follows a list of causes of troponin elevation.
- Acute myocardial infarction (STEMI, NSTEMI)
- Cardiac contusion/trauma
- Acute heart failure or chronic heart failure
- Takotsubo cardiomyopathy
- Perimyocarditis (myocarditis, pericarditis)
- Cardiac procedures
- CABG
- PCI
- Ablation
- Implantation of pacemaker, ICD or CRT
- Electrical cardioversion
- Myocardial biopsy
- Supraventricular tachyarrhythmia (e.g atrial fibrillation)
- Ventricular tachyarrhythmia (e.g. ventricular tachycardia)
- Hypertensive crisis
- Stroke or subarachnoid hemorrhage
- Intoxication
- Extreme physical exertion
- Aortic dissection
- Valvular heart disease (e.g aortic stenosis, aortic insufficiency)
- Rhabdomyolysis with cardiac injury
- Pulmonary embolism
- Severe pulmonary hypertension
- Renal failure
- Critically ill patients (e.g sepsis, burns, etc)
- Hypothyroidism
- Hyperthyroidism
- Amyloidosis
- Hemochromatosis
- Sarcoidosis
- Scleroderma
- Cardiotoxic drugs (doxorubicin, 5-fluorouracil, herceptin)
Rule in and rule out algorithms
The ESC (European Society for Cardiology) advocates the use of early rule out and rule in algorithms. These algorithms have been extensively validated in prospective studies and randomized clinical trials, with all major troponin assays. The algorithms are used in the emergency room to rule in or rule out myocardial infarction. The ESC currently recommends the 0 h / 1 h algorithm, which is currently used in the majority of North America, European and Asian hospitals. The algorithms have very high sensitivity for acute myocardial infarction.
Troponin algorithms are not used in patients presenting with ST-segment elevation on ECG. These patients are managed with a primary PCI strategy, meaning that they undergo urgent angiography with readiness to perform PCI.
Nurses should obtain troponin measurements immediately on patient arrival (t = 0 h) and after 1 h (± 10 minutes), regardless of patient characteristics.
The decisions in the algorithms are based on whether the troponin level is very low, low, high, or if a change (Δ) occurs during repeated measurements after 1, 2 or 3 hours. Each assay has defined the cut-offs for these values, as visible in Table 1.
Table 1. Assay-specific cut-offs for troponin levels
| 0 h/1 h algorithm | Very low | Low | No 1 h change (1hΔ) | High | 1hΔ |
| hs-cTn T (Elecsys; Roche) | <5 | <12 | <3 | ≥52 | ≥5 |
| hs-cTn I (Architect; Abbott) | <4 | <5 | <2 | ≥64 | ≥6 |
| hs-cTn I (Centaur; Siemens) | <3 | <6 | <3 | ≥120 | ≥12 |
| hs-cTn I (Access; Beckman Coulter) | <4 | <5 | <4 | ≥50 | ≥15 |
| hs-cTn I (Clarity; Singulex) | <1 | <2 | <1 | ≥30 | ≥6 |
| hs-cTn I (Vitros; Clinical Diagnostics) | <1 | <2 | <1 | ≥40 | ≥4 |
| hs-cTn I (Pathfast; LSI Medience) | <3 | <4 | <3 | ≥90 | ≥20 |
| hs-cTn I (TriageTrue; Quidel) | <4 | <5 | <3 | ≥60 | ≥8 |
| 0 h/2 h algorithm | Very low | Low | No 2 h change (2hΔ) | High | 2hΔ |
| hs-cTn T (Elecsys; Roche) | <5 | <14 | <4 | ≥52 | ≥10 |
| hs-cTn I (Architect; Abbott) | <4 | <6 | <2 | ≥64 | ≥15 |
| hs-cTn I (Centaur; Siemens) | <3 | <8 | <7 | ≥120 | ≥20 |
| hs-cTn I (Access; Beckman Coulter) | <4 | <5 | <5 | ≥50 | ≥20 |
| hs-cTn I (Clarity; Singulex) | <1 | TBD | TBD | ≥30 | TBD |
| hs-cTn I (Vitros; Clinical Diagnostics) | <1 | TBD | TBD | ≥40 | TBD |
| hs-cTn I (Pathfast; LSI Medience) | <3 | TBD | TBD | ≥90 | TBD |
| hs-cTn I (TriageTrue; Quidel) | <4 | TBD | TBD | ≥60 | TBD |
0 h / 1 h algorithm
The flowchart below shows how the 0 h / 1 h algorithm. Troponin is analyzed at 0 h (on arrival) and at 1 h. According to the ESC, this is the best method and it should be preferred over the 0 h / 2 h and 0 h / 3 h algorithms (Wildi et al).
The same principle is applied for the 0 h / 2 h algorithm, but with different cut-offs according to Table 1.
Cardiac troponin in sudden cardiac arrest
Cardiac-specific Troponin T (TnT) and Troponin I (TnI) are often analyzed in cases of out-of-hospital cardiac arrest to determine whether the cardiac arrest was caused by an acute myocardial infarction. The rationale behind this is that myocardial necrosis commences after 20 minutes of complete myocardial anoxia. Thus, cardiac arrests due to causes other than acute myocardial infarction should present with low levels of troponins, as opposed to infarction-caused cardiac arrests, which should result in high troponin levels. However, it is questionable whether troponin can be used for this purpose. In a study of 145 patients who regained circulation after cardiac arrest and underwent serial troponin measurements and echocardiographic examinations, all individuals had elevated troponin levels. Therefore, troponin levels could not be used to distinguish infarction-related cardiac arrest from other causes. Troponin levels also did not correlate with survival or left ventricular function (Agusala et al.).
References
2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Jean-Philippe Collet, Holger Thiele, Emanuele Barbato, Olivier Barthélémy, Johann Bauersachs, Deepak L Bhatt, Paul Dendale, Maria Dorobantu, Thor Edvardsen, Thierry Folliguet et al. European Heart Journal (2020).
Rubini Gimenez M, Twerenbold R, Reichlin T, et al. Direct comparison of high-sensitivity-cardiac troponin I vs. T for the early diagnosis of acute myocardial infarction. Eur Heart J. 2014 Sep 7;35(34):2303-11.
Gore MO, Seliger SL, Defilippi CR, et al. Age- and sex-dependent upper reference limits for the high-sensitivity cardiac troponin T assay. J Am Coll Cardiol. 2014 Apr 15;63(14):1441-8.
Lee KK, Ferry AV, Anand A, et al; High-STEACS Investigators. Sex-Specific Thresholds of High-Sensitivity Troponin in Patients With Suspected Acute Coronary Syndrome. J Am Coll Cardiol.2019 Oct 22;74(16):2032-2043.
Mueller T, Egger M, Peer E, et al. Evaluation of sex-specificcut-off values of high-sensitivity cardiac troponin I and T assays in an emergency department setting – Results from the Linz Troponin (LITROP) study. Clin Chim Acta. 2018 Dec;487:66-74.
Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019;40:237-69.
Shah ASV , Anand A , Strachan FE , Ferry AV , Lee KK , Chapman AR , Sandeman D , Stables CL , Adamson PD , Andrews JPM , Anwar MS , Hung J , Moss AJ , O’Brien R , Berry C , Findlay I , Walker S , Cruickshank A , Reid A , Gray A , Collinson PO , Apple FS , McAllister DA , Maguire D , Fox KAA , Newby DE , Tuck C , Harkess R , Parker RA , Keerie C , Weir CJ , Mills NL , High-STEACS investigators. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet 2018;392:919–928.
Wildi K, Nelles B, Twerenbold R, Rubini Gimenez M, Reichlin T, Singeisen H, Druey S, Haaf P, Sabti Z, Hillinger P, Jaeger C, Campodarve I, Kreutzinger P, Puelacher C, Moreno Weidmann Z, Gugala M, Pretre G, Doerflinger S, Wagener M, Stallone F, Freese M, Stelzig C, Rentsch K, Bassetti S, Bingisser R, Osswald S, Mueller C. Safety and efficacy of the 0 h/3 h protocol for rapid rule out of myocardial infarction. Am Heart J 2016;181:16–25.
Unstable angina: is it time for a requiem? Eugene Braunwald, David A Morrow. Circulation . 2013 Jun 18;127(24):2452-7. doi: 10.1161/CIRCULATIONAHA.113.001258.
