Digoxin – ECG changes, arrhythmias, conduction defects & treatment
Digoxin ECG changes: arrhythmias, conduction defects and waveform changes
Digoxin may be used in patients with heart failure, atrial fibrillation, atrial flutter, and in selected cases of paroxysmal supraventricular tachycardia. Due to its profound pro-arrhythmic effects and lack of compelling data regarding morbidity and mortality benefits, digoxin has been ousted repeatedly from the standard of care for these conditions. However, digoxin is still used in patients who do not achieve satisfactory effects using first-line therapies. Digoxin is also used frequently in the emergency setting to control ventricular rate during supraventricular tachycardias (e.g. atrial fibrillation). Because digoxin may cause life-threatening arrhythmias, every healthcare provider must be able to recognize common digoxin ECG changes and arrhythmias.
Digoxin effects on cardiac function and ECG
Digoxin has a positive inotropic effect and a negative chronotropic effect, enhancing ventricular contractility while lowering heart rate. The positive inotropic effect is due to the inhibition of the sodium-potassium adenosine triphosphatase (NaK-ATPase) in the ventricular myocardium. Inhibition of Na-K-ATPase leads to an increase in intracellular concentration of sodium, which affects the sodium-calcium exchanger such that ultimately intracellular calcium concentration increases. This makes more calcium available to the contractile proteins which therefore produce stronger contractions. Lowering of the heart rate is due to increased Vagus nerve activity caused by digoxin. Increased Vagus activity diminishes the automaticity in the sinoatrial node (which lowers heart rate) and also slows conduction over the atrioventricular (AV) node.
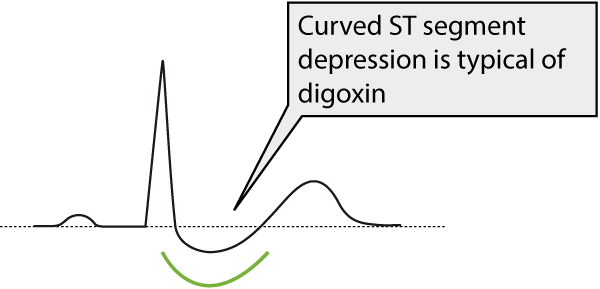
The most classical ECG finding is generalized ST segment depressions with curved ST segment (generalized implies that the depressions may occur in most ECG leads). Refer to Figure 1.
Adverse effects of digoxin
The incidence of adverse drug reactions is high, owing to the narrow therapeutic index of the drug. Digoxin is significantly pro-arrhythmic, increasing the probability of arrhythmias occurring. This is explained by the increase in intracellular calcium levels, which causes a shortening of the action potential. Digoxin shortens the action potential in all cardiac cells, both in the atria and the ventricles. This increases the automaticity in cells with natural automaticity but it may also provoke abnormal automaticity in cells that normally do not exhibit automaticity. The effect on automaticity should be distinguished from the effect on impulse conduction because digoxin slows impulse conduction.
It is important to note that the association between ECG changes and the risk of arrhythmia is weak. Hence, arrhythmias may occur in the absence of ECG changes and vice versa (i.e. ECG changes may be pronounced without any arrhythmias occurring). Plasma levels >2 ng/mL are considered an overdose. However, arrhythmia may occur at plasma levels below 2 ng/mL and arrhythmias may not occur even at higher plasma levels. Thus, digoxin is rather unpredictable in terms of arrhythmia risk.
Hypokalemia potentiates the digoxin effect
Hypokalemia always potentiates the pro-arrhythmic effects of digoxin. Potassium levels must always be assessed in patients using digoxin whenever they seek medical attention. Arrhythmias may occur already at therapeutic plasma levels of digoxin in the setting of hypokalemia.
Arrhythmias caused by digoxin
Digoxin may cause virtually all known arrhythmias. However, none of the ECG changes or arrhythmias are unique to digoxin. One should always suspect digoxin as the trigger of an arrhythmia (in patients using digoxin) if there is evidence of increased automaticity and diminished impulse conduction. Explanation follows:
- Increased automaticity occurs both in the atria and the ventricles. This initially manifests with premature beats (premature atrial beats or premature ventricular beats), which are considered an early sign of overdosing. At higher plasma levels atrial tachyarrhythmias and ventricular tachyarrhythmias may occur. Junctional tachycardia is less common. Ventricular arrhythmias generally occur at higher plasma levels.
- Diminished impulse conduction may manifest as lengthening of the PR interval, atrioventricular (AV) block (which is usually heart rate dependent), or sinoatrial (SA) block (which is usually transient).
The typical patient with digoxin overdose will present with extrasystoles (premature beats) and various degrees of AV block.
A rather peculiar form of ventricular tachycardia may occur in digoxin intoxication, namely bidirectional ventricular tachycardia. This type of ventricular tachycardia exhibits an electrical axis shifting from left to right from one beat to the next. Figure 2 (Szentpali et al) shows an example of bidirectional ventricular tachycardia.
Table 1. Digoxin effects on rhythm and conduction
| Effect on sinoatrial (SA) node | Digoxin enhances Vagus nerve activity which decreases the automaticity in the SA node. |
| P-wave | No clinically significant effect. |
| AV system (AV node, His bundle, Purkinje system) | Digoxin enhances Vagus nerve activity, which slows conduction over the AV node. Digoxin also has a direct effect on AV conduction, by slowing it. This causes prolongation of the PR interval, which is considered a normal finding, unless severely prolonged. Second- and third-degree AV block is evidence of intoxication. Automaticity is increased in the entire AV system (AV node, His bundle, Purkinje fibers). |
| QRS complex | No effect |
| ST segment | ST segment depression with a curved appearance (Figure 1). |
| T-wave | The T-wave amplitude typically diminishes. The initial portion of the T-wave may be negative but the latter portion is mostly positive (thus the T-wave may appear biphasic/diphasic). The T-wave may become completely inverted (negative) as well. The latter is more common in overdose. |
| U-wave | Increased amplitude |
| QT (QTc) interval | Shortening of the QT interval occurs at therapeutic doses. |
| Arrhythmia | Digoxin is extremely pro-arrhythmogenic and may cause virtually all known arrhythmias and conduction defects. The arrhythmias/conduction defects that are not caused by digoxin are as follows: second-degree AV block type 2, atrial flutter, bundle branch block. One should be particularly suspicious if there is evidence of increased automaticity and simultaneous diminished impulse conduction (e.g AV block). Ventricular premature beats are common. They indicate an increased risk of ventricular tachycardia, idioventricular rhythm and ventricular fibrillation. Ventricular beats may be unifocal or multifocal. They commonly occur in bigemini or trigemini. AV blocks are also very common, as is atrial fibrillation. |