Approach to patients with chest pain: differential diagnoses, management & ECG
Approach to patients with chest pain: differential diagnoses, evaluation and management
Chest pain is one of the most common symptoms in the emergency department, as well as in primary health care. The cause (etiology) of chest pain varies according to age, sex, risk factors, type of symptoms etc. Chest pain is actually one of the most nuanced symptoms in clinical practice and it is fundamental to be able to differentiate benign from serious etiologies. Therefore, when encountering a patient with chest pain the primary task is to exclude or verify the following potentially life-threatening causes of chest pain:
- Ischemic heart disease: stable angina pectoris, unstable angina pectoris, acute myocardial infarction (AMI). Note that unstable angina pectoris and acute myocardial infarction are categorized under acute coronary syndromes (ACS).
- Aortic dissection
- Pneumothorax
- Pulmonary embolism
- Mediastinitis (rare condition)
In addition to these five conditions, there are numerous other causes of chest pain, but the other causes are either subacute or non-acute. It is important that the history taking is systematic and accurate because the history itself is often sufficient to make a diagnosis or identify a few likely diagnoses. The table below shows a systematic history taking in patients presenting with chest pain (chest discomfort) or other symptoms suggestive of the five conditions listed above. It is important that history taking and physical examination is carried out systematically and carefully without delaying time to treatment.
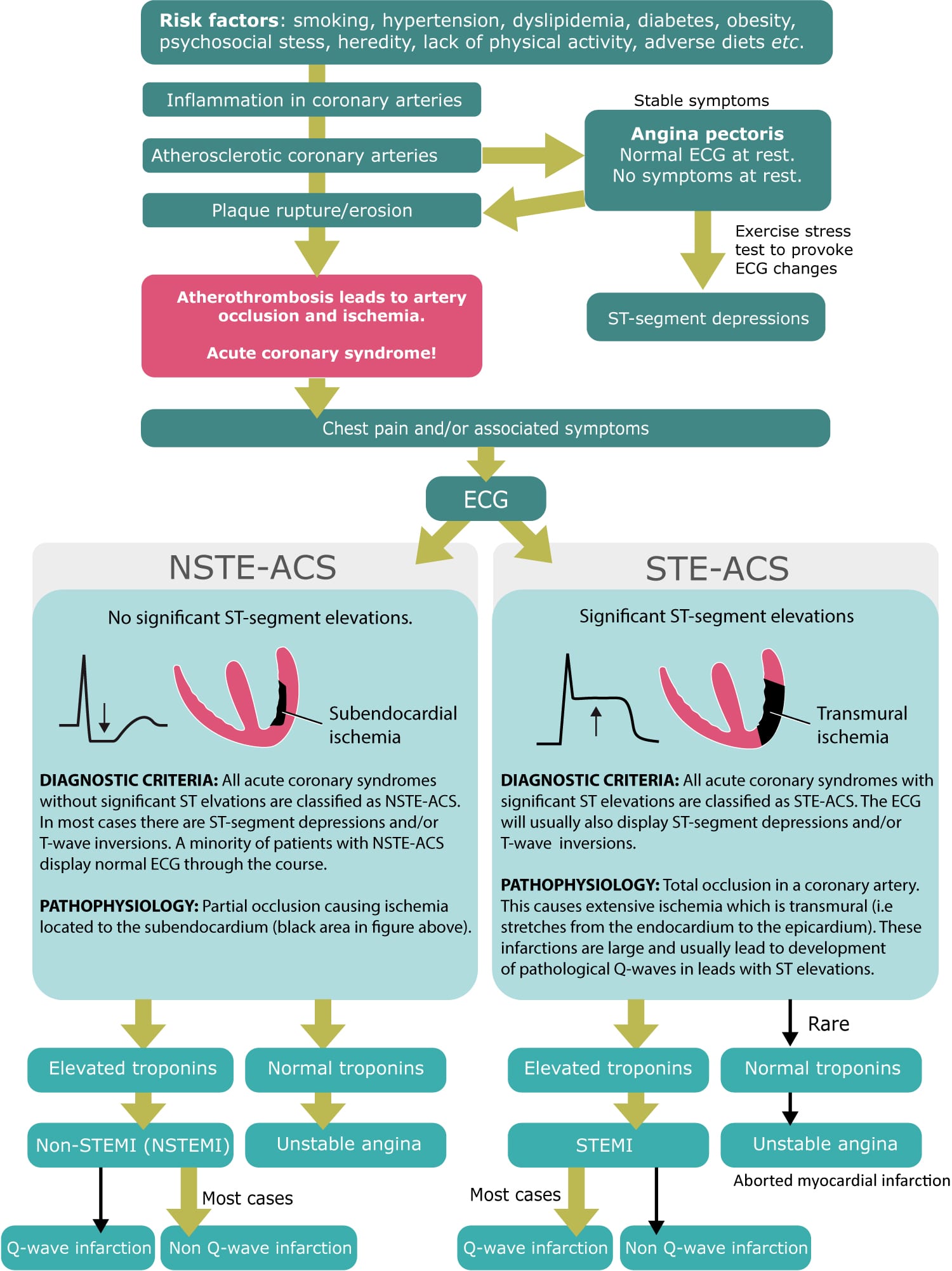
History taking, physical examination, ECG and laboratory tests are the cornerstones of management of patients with chest pain. A 12-lead ECG recording must be registered and interpreted within 10 minutes of arrival to the hospital. The ECG differentiates between ST elevation acute coronary syndromes (STE-ACS) and non-ST elevation acute coronary syndromes (NSTE-ACS). The division into STE-ACS and NSTE-ACS has profound implications for management and treatment of patients with acute coronary syndromes. Moreover, clinicians must clarify whether the ECG was recorded during chest pain, since an ECG without signs of ischemia during chest pain in principle excludes myocardial ischemia as the cause of the pain. Refer to The ischemic cascade for details.
History taking in patients with chest pain (chest discomfort)
| HISTORY PARAMETER | QUESTIONS | COMMENTS |
|---|---|---|
| Risk factors for the 5 serious etiologies | Family history (focus on ischemic heart disease, aortic dissection, pulmonary embolism, pneumothorax). Hypertension. Smoking. Dyslipidemia (hyperlipidemia). Obesity and/or diabetes. Psychosocial stress. Alcohol abuse. Physical inactivity. Unhealthy diet. Cerebral / peripheral vascular disease. Cancer. | All these risk factors (except from cancer) are associated with the risk of ischemic heart disease (including acute coronary syndromes). Risk factors for aortic dissection are similar to ischemic heart disease. Pulmonary embolism is frequently caused by cancer. |
| Triggering factors | Symptoms triggered by exercise/effort (what level of exercise)? Symptoms at rest? Symptoms more easily provoked after a meal? Symptoms provoked by (or after a period of) stress? Symptoms related to body position or respiration? | Acute coronary syndromes cause symptoms already at rest. Stable ischemic heart disease do not cause symptoms at rest unless the stenosis is so grave that myocardial oxygen demands cannot be satisfied even at rest. Ischemic chest pain is more easily provoked after a meal because food intake redistributes blood to the gastrointestinal tract which reduces blood availability in the heart. Symptoms of ischemic heart disease are generally not related to body position or respiration. |
| Onset and evolution | How do symptoms start (suddenly or gradually)? When did the patient first note the symptoms and how have the symptoms developed over time? | In stable ischemic heart disease, symptoms are typically not present at rest but they occur during exercise when the oxygen demand in the myocardium is increased. Ischemic chest pain typically has a gradual onset, reaching a maximum within a few minutes and if the pain subsides, it does so gradually. Some patients with acute coronary syndromes have an established diagnosis of ischemic heart disease, while others have never had any symptoms prior to developing the acute coronary syndrome. In stable ischemic heart disease, the symptoms tend to worsen over time, meaning that they arise at lower levels of exercise and are more severe. This usually takes months or years to develop. |
| Localization of pain | Where is the pain located? Diffuse or distinct location? Pain radiating to the left? More severe on the left side? | Ischemic heart disease typically causes diffuse pain over a wide area of the anterior chest wall (the pain is not localized). Ischemic heart disease also tends to cause pain radiating to the left arm, neck, shoulder or jaw. Patients typically report that the pain is more severe on the left side of the chest. |
| Pain quality | Describe the type of pain (pressure/cramp/crushing, cutting, burning etc). | Ischemic chest pain is usually described as pressure, squeezing, or a crushing sensation across the precordium and may radiate to the neck, shoulder, jaw, back, upper abdomen, left or right arm. |
| Associated symptoms | Pain radiation to arm, neck, jaw or back? Cold sweats? Anxiety? Nausea or vomiting? Presyncope / syncope? Palpitations? Dyspnea? Reflux? Fever? | Ischemic chest pain causes symptoms from the autonomic nervous system, most notably diaphoresis (sweating), nausea, and vomiting. Dyspnea suggests either a cardiac or pulmonary etiology. Presyncope/syncope suggests either a cardiac or pulmonary etiology. Palpitations suggest either a cardiac or pulmonary etiology. |
| Alleviating factors | Pain alleviated by rest? Pain alleviated by nitroglycerin? | Ischemic chest pain is typically alleviated by rest and by administration of nitroglycerin. However, these characteristics are not specific to ischemic chest pain. |
| Frequency of symptoms | How many episodes of chest pain? When was the worst / longest episode and its duration? Increased frequency and/or intensity last month? Time of the latest episode? | Myocardial infarction occurs after 20 minutes of severe ischemia. It may take up to 6 hours for troponin levels to increase significantly after myocardial infarction, which is why troponin results are not conclusive before 6 hours after the last episode of pain. Thus, if 6 hours have passed since the last episode of pain, the troponin tests will be able to determine whether the patient developed myocardial infarction. In patients with stable ischemic heart disease, increased frequency and/or intensity of the symptoms the last month suggests that they have developed unstable angina pectoris (which is an acute coronary syndrome). |
| Other | Recent infections (particularly airway infection)? Chest trauma? Heavy physical exertion? | All these suggest non-ischemic causes. |
| Alarming signs | Severe pain. Affected general appearance. Cutting pain and/or back pain. Morphine-resistant pain. Diabetics, elderly and women. Epigastralgia. Pulmonary edema. | Severe pain increases the likelihood of serious etiologies. If the patient’s general appearance is affected, it increases the likelihood of serious etiologies. Cutting pain and/or back pain (particularly if it has migrated down along thorax) suggests aortic dissection. Morphine-resistant pain suggests serious etiologies. Diabetics, elderly and women may have atypical symptoms, which is why angina equivalents (dyspnoea, sweating, extreme fatigue, atypical pain) must be assessed. In elderly dyspnoea is as common as angina in acute myocardial infarction. Note that epigastralgia may be caused by inferior myocardial infarction. Pulmonary edema. |
The severity of symptoms in patients with angina pectoris should be graded according to the Canadian Cardiovascular Society (CCS):
| Grade I | Ordinary physical activity does not cause angina, such as walking and climbing stairs. Angina with strenuous or rapid or prolonged exertion at work or recreation. |
| Grade II | Slight limitation of ordinary activity. Walking or climbing stairs rapidly, walking uphill, walking or stair climbing after meals, or in cold, or in wind, or under emotional stress, or only during the few hours after awakening. Walking more than two blocks on the level and climbing more than one flight of ordinary stairs at a normal pace and in normal conditions. |
| Grade III | Marked limitation of ordinary physical activity. Walking one or two blocks on the level and climbing one flight of stairs in normal conditions and at normal pace. |
| Grade IV | Inability to carry on any physical activity without discomfort, anginal syndrome may be present at rest. |
Characteristics of various causes of chest pain
Ischemic chest pain: angina pectoris and acute coronary syndromes
Ischemic chest pain causes diffuse discomfort over a wide area of the anterior chest wall. The pain is typically not localized and is described as a pressure, cramp or crushing sensation. The pain may radiate to either arm, neck, back or shoulder. Radiation to the arms rarely reaches the fingertips. These symptoms are more severe when the ischemia causes myocardial infarction. Shortness of breath (dyspnea) frequently accompanies chest discomfort and some patients may have difficulties discerning these symptoms.
Several factors influence the symptoms presented. Women, elderly and persons with diabetes frequently present with atypical symptoms; notably, these three groups may present with only dyspnea. In fact, in the elderly with acute myocardial infarction, dyspnea is as common as chest discomfort. Moreover, women with acute myocardial infarction report back pain, neck pain and jaw pain more often than males.
Stable angina pectoris and acute coronary syndromes differ in several aspects, which are now clarified.
- Angina pectoris: Angina pectoris is a diffuse pain over the anterior chest wall. It is described as a pressure, cramp or crushing sensation. Angina pectoris is diagnosed when the ischemic heart disease is stable, which implies that symptoms only appear in situations with increased myocardial workload, and symptoms subside when the workload returns to normal. The most typical scenario is angina pectoris provoked by exercise and mental stress. Both these scenarios increase heart rate and workload which subsequently causes ischemia. However, in stable angina pectoris, the symptoms must subside within minutes after resting or after administration of nitroglycerin. Otherwise, the condition is not stable. Angina pectoris is more easily provoked by cold. Some patients have angina pectoris due to coronary artery vasospasm, but this is considerably less common than atherosclerosis.
- Unstable angina pectoris: Unstable angina pectoris is defined as angina pectoris that has changed and become aggravated recently (up to 30 days). Three scenarios are typically defined as unstable angina pectoris: (1) angina pectoris at rest, or with minimal exertion, lasting 10 minutes or longer; (2) new-onset angina with severe pain; (3) angina pectoris which has worsened by becoming more frequent, more severe and with longer duration. Nitroglycering has insufficient effect. Patients with unstable angina pectoris are at considerable risk of developing acute myocardial infarction. Unstable angina pectoris and all types of acute myocardial infarction are categorized as acute coronary syndromes (ACS); their underlying etiology is the same, namely a ruptured atherosclerotic plaque.
- Acute myocardial infarction (AMI): The pain is similar to unstable angina pectoris but more severe. Duration is virtually always longer than 15 minutes but shorter than 12 hours. Autonomic symptoms such as nausea, diaphoresis etc are very common.
Classification of acute coronary syndromes (acute myocardial infarction) is presented in the following figure.
Pericarditis and perimyocarditis
- Pericarditis may also cause chest pain on the anterior chest wall; the pain area varies from the size of a coin to a hand.
- The pain is often correlated with respiration. Deep breaths typically aggravate the pain.
- The pain is often alleviated by leaning forward or to the left side.
- The intensity of the pain may very well be equal to the pain in ACS.
Gastrointestinal chest pain
- May also be located on the anterior chest wall.
- Described as a pressure or burning sensation.
- Can be aggravated by physical exertion and alleviated by food intake.
- Nitroglycerin may relieve the pain caused by esophageal spasms.
- Gastric ulcers are relieved by acid inhibitors.
- Reflux esophagitis is relieved by standing up or drinking milk.
- Esophagitis and esophageal spasm may mimic the pain in myocardial ischemia.
Pulmonary chest pain
- A large pneumonia causes chest pain correlated with respiration.
Musculoskeletal chest pain
- Musculoskeletal chest pain may be located anywhere on the chest wall and back.
- The pain is usually sharp, typically related to body position and intermittent.
- Tietze’s syndrome should be considered. It is a benign inflammation of one or more of the costal cartilages. The chest pain is accompanied by tenderness and swelling of the affected cartilages. The cartilages are usually tender upon palpation and the pain is aggravated with respiration. Although it may be very painful, Tietze’s Syndrome is considered to be a benign syndrome that generally resolves in 3 months.
- Spondylitis may cause back pain if located in the thoracic vertebrae.
- Rib fractures cause located chest pain which correlates with respiration. Palpation provokes severe pain. The pain subsides gradually within 3 weeks.
Vascular chest pain (aortic dissection)
Aortic dissection may sometimes present with symptoms that are indistinguishable from acute myocardial infarction. Symptom presentation also depends on where the dissection originates and whether it continues to dissect. The pain is, as compared with acute myocardial infarction, more often described as a tearing, ripping or shearing pain that radiates to the neck or down the back. The pain is very severe and resistant to morphine unless high doses are administered. Shortness of breath is very common as are autonomic symptoms such as paleness, diaphoresis and nausea. Notably, neurological symptoms are rather specific to aortic dissection; the dissection may cause occlusion of large arteries supplying both the cerebral, abdominal and extremities circulation. Thus, neurological, abdominal and peripheral pain may be seen during aortic dissection.
Cardiac neurosis
Anxiety and stress may cause chest pain. Many individuals with chest are worried their symptoms may be caused by myocardial infarction, which further exacerbates their symptoms. The pain is usually located to the left and it is aggravated during periods of stress or anxiety. Frequently the pain has a fairly precise location to the left; patients tend to point with a finger towards the location of the pain. The symptoms are not related to exercise. Some patients also experience palpitations, hyperventilation, dyspnea and irregular heartbeats.
Physical examination
A complete physical examination is always warranted. Emphasis should, however, be put on the following parameters:
- General appearance – Any sign of affected general appearance may indicate that the underlying cause is serious.
- Heart rate – The heart rate does not distinguish between the differential diagnoses, but it must be assessed to evaluate circulatory status.
- Blood pressure – The blood pressure should be measured in both arms if there is suspicion of aortic dissection. A difference in pressure (between the left and right arm) greater than 15 mmHg increases the suspicion of aortic dissection.
- Oxygen saturation
- Respiratory rate
- Body temperature
- Signs of incompensation (heart failure)
- Inspect and palpate the thoracic wall. Clarify whether the pain is related to palpation, rotation of the torso or any other body position, arm movements etc.
ECG (EKG) changes in ischemia/infarction
ECG changes in myocardial ischemia and infarction have already been discussed. Briefly, the following ECG changes suggest myocardial ischemia or infarction.
- ST segment elevation (STEMI)
- ST segment depression (NSTEMI)
- T-wave changes: flat T-waves, inverted T-waves, hyperacute T-waves
- Pathological Q-waves, QS complex, Pathological R-wave progression, Fragmented QRS segment
- New left bundle branch block (LBBB)
- New arrhythmias (both bradycardia and tachycardia)
- New conduction defects
If possible, the ECG should be recorded during ongoing chest pain. The reason for this is that chest pain that does not provoke ischemic ECG changes is not caused by myocardial ischemia/infarction (please refer to The ischemic cascade). Thus, an ECG with no signs of ischemia, recorded during chest pain, excludes myocardial ischemia as the underlying cause of the symptoms. Moreover, it is important to compare the current ECG with a previous recording, if such is available.
It is recommended that the ECG be repeated at 5–15 minutes intervals (even in the emergency room). Myocardial ischemia is a dynamic process and 60% of the ischemic episodes that are detected with ECG are asymptomatic.
Also consider additional ECG leads if there is suspicion of posterior (posterolateral) myocardial infarction or right ventricular infarction.
Laboratory tests
Troponin T or troponin I is used to detecting myocardial necrosis (refer to Diagnostic criteria for acute myocardial infarction). It may take up to 6 hours for troponin levels to increase significantly after acute myocardial infarction. Thus, troponin samples are not conclusive until 6 hours after the last episode with chest pain. In clinical practice, troponin samples are taken on arrival and 6 hours later. A third sample may be taken 24 hours after survival. Blood lipids and glucose must always be analysed. D dimer is only analysed if there is suspicion of pulmonary embolism.
Radiological examinations
Chest X ray is generally not indicated. However, it may be considered if there is suspicion of pneumothorax, pleuritis, pneumonia or heart failure.
Computerized tomography (CT) is indicated if there is suspicion of aortic dissection or pulmonary embolism. Modern CT protocols are capable of elucidating both these differential diagnoses.
Echocardiogram, including assessment of the aorta, is recommended and may guide both diagnostics and therapy.
Risk stratification of patients with acute coronary syndromes (ACS)
Use evidence-based risk models to estimate the risk of infarction and death.
- GRACE: www.outcomes-umassmed.org/grace
- TIMI: www.timi.org

