Ectopic atrial rhythm (EAT), atrial tachycardia (AT) & multifocal atrial tachycardia (MAT)
Atrial rhythms: ectopic atrial rhythm, atrial tachycardia and multifocal atrial tachycardia
Ectopic atrial tachycardia (EAT, or atrial tachycardia) arises when an ectopic focus within the atria generates electrical impulses at a rate exceeding that of the sinoatrial (SA) node. This enhanced atrial activity is most commonly attributable to abnormal automaticity or re-entry mechanisms; triggered activity is a less frequent cause. The atrial rate typically ranges from 120 to 250 beats per minute. To fulfill the diagnostic criteria for EAT, the ventricular rate must exceed 100 beats per minute. When the ventricular rate remains below this threshold, the arrhythmia is classified instead as an ectopic atrial rhythm (EAR).
Ectopic atrial tachycardia (EAT) most commonly occurs in individuals with underlying structural or electrical heart disease. Less frequently, it may also present in individuals without identifiable cardiac disease. Contributing factors include pulmonary disorders, particularly obstructive pulmonary disease, the use of theophylline, and elevated catecholamine states. EAT typically has an abrupt onset, although a brief warm-up phase lasting approximately 5 to 10 seconds may precede the full tachycardia. It is characterized by short, rapid bursts of atrial activity. In the majority of cases, the arrhythmia is self-limiting; however, it may recur and, in some instances, persist for extended durations. As for any long-standing tachycardia, there is a risk of developing tachycardia-induced cardiomyopathy.
In pediatric populations, a distinct form of atrial tachycardia may occur due to embryological remnants within the atrial myocardium. These residual tissues, persisting from cardiac embryogenesis, are capable of exhibiting markedly increased automaticity, thereby serving as ectopic pacemaker foci.
The term “ectopic” is often omitted in clinical practice, and these arrhythmias are commonly referred to simply as atrial tachycardia or atrial rhythm, depending on the ventricular response.
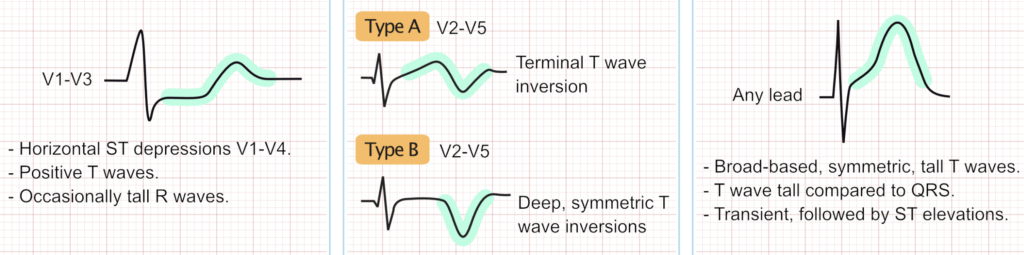
The ECG in ectopic atrial rhythm and atrial tachycardia
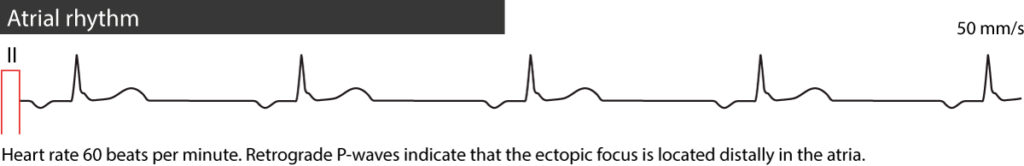
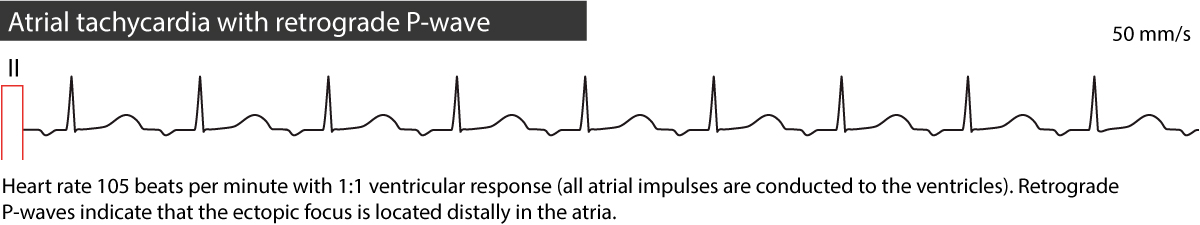
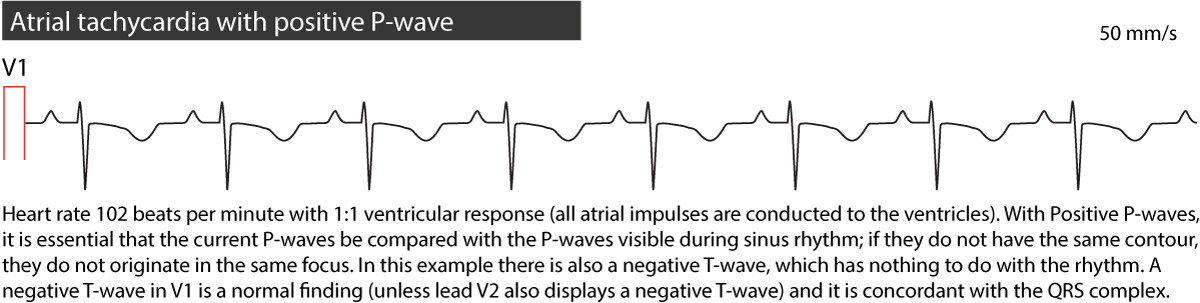
- A regular rhythm with P-waves that differ in contour from sinus P-waves. If the P-waves in lead II are retrograde (negative), the diagnosis is straightforward, as sinus P-waves are never negative in this lead. When P-waves are positive in lead II, comparison of P-wave morphology during tachycardia and sinus rhythm is typically required.
- The isoelectric baseline lacks the saw-tooth pattern characteristic of atrial flutter.
- Each P-wave is followed by a QRS complex; atrioventricular block is uncommon unless the patient is receiving digoxin.
- The ventricular rate is regular, typically ranging from 100 to 250 beats per minute in atrial tachycardia and less than 100 beats per minute in atrial rhythm.
Refer to ECG examples in Figures 1, 2 and 3 below.
Causes of ectopic atrial tachycardia and ectopic atrial rhythm
- Side effect of digoxin.
- Heart failure.
- Lung disease (COPD, pulmonary hypertension, etc).
- Ischemic heart disease (coronary artery disease).
- Structural heart disease, any.
Treatment of atrial tachycardia
Discontinuation of digoxin is typically sufficient in patients whose atrial tachycardia is induced by the drug. Management of all other cases aligns with the approach used for atrial fibrillation and atrial flutter. Beta-blockers, digoxin, and calcium channel blockers may be used to control the ventricular rate. If rate control is inadequate, the use of Class IA, IC, or III antiarrhythmic agents may be considered. Catheter ablation should be considered in patients with a high risk of recurrence. Electrical cardioversion is generally ineffective in the treatment of atrial tachycardia.
Multifocal atrial tachycardia
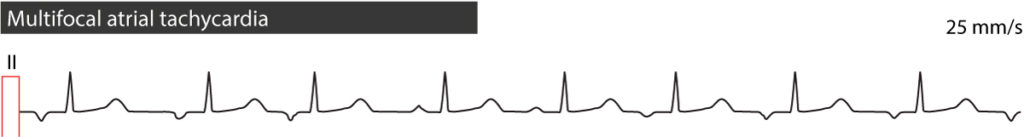
Multifocal atrial tachycardia is an uncommon variant of ectopic atrial tachycardia. As illustrated in Figure 4, it is characterized by an irregular rhythm with clearly discernible P-waves (unlike atrial fibrillation) while the morphology of the P-waves varies from beat to beat. This variability is due to the presence of multiple ectopic atrial foci generating impulses that activate the atria. The arrhythmia typically has a gradual onset. In most cases, there is a 1:1 atrioventricular conduction, meaning each atrial impulse is conducted to the ventricles. The ventricular rate usually ranges between 100 and 150 beats per minute.
Multifocal atrial tachycardia may be intermittent with intervening periods of sinus rhythm. The most common underlying causes are heart failure, atrial ischemia, increased atrial pressure, use of theophyllamine or chronic lung disease (particularly COPD). Multifocal atrial tachycardia may occur in children.
Note that if the atrial rhythm is below 100 beats per minute, it is referred to as multifocal atrial rhythm.
Treatment of multifocal atrial tachycardia
Treatment should be directed toward correcting the underlying cause, as resolution of the precipitating factor often leads to spontaneous termination of the arrhythmia. Electrical cardioversion is contraindicated as it is ineffective and may potentially exacerbate the arrhythmia. Beta-blockers are generally considered the first-line pharmacologic option, provided there are no contraindications such as significant pulmonary disease. The efficacy of conventional antiarrhythmic agents is limited, though diltiazem, verapamil, and amiodarone may be considered in selected cases. In addition, magnesium and potassium supplementation is recommended as part of supportive management.