Evaluation and management of stable coronary artery disease
Chronic coronary syndromes (CCS)
Stable coronary artery disease (CAD), frequently referred to as stable angina pectoris, has traditionally been defined and managed as a distinct clinical entity. The hallmark of stable coronary artery disease is exercise-related angina pectoris (chest pain); symptoms of ischemia appear during circumstances with increased myocardial demand, typically exercise. Recent guidelines issued by the European Society for Cardiology (ESC) suggest a new classification (Knuuti et al, 2019/2020), in which stable coronary artery disease is part of the broader syndrome of chronic coronary syndromes (CCS). This syndrome includes six clinical manifestations of coronary artery disease (discussed below). Moreover, prognostication, selection of diagnostic tests, and treatment strategies have been updated. For example, exercise stress testing is no longer recommended in the initial evaluation of patients with suspected coronary artery disease (i.e CCS).
The new guidelines are based on data derived from studies conducted mainly in North America and Europe. Moreover, the guideline committee included representatives from North America, making it very likely that the coming guidelines by the American Heart Association (AHA) and American College of Cardiology (ACC) will be in line with the European guidelines. Hence, this chapter will present the most recent evidence and recommendations for the evaluation and treatment of chronic coronary syndromes (CCS).
Ischemic heart disease, coronary heart disease (CAD) and coronary artery disease (CHD) are synonyms. These terms refer to symptomatic coronary atherosclerosis.
Traditional classification of coronary artery disease
Traditionally, coronary artery disease has been classified into the following three syndromes:
- Stable angina pectoris: Symptoms appear primarily during exercise or other situations with increased myocardial load. Symptoms are exacerbated by increasing the level of exertion (i.e increasing the myocardial load), and vice versa. Stable angina pectoris is a chronic and mostly progressive disease.
- NSTE-ACS (Non-ST Elevation Acute Coronary Syndrome): NSTE-ACS is an acute condition that occurs when an atherosclerotic plaque ruptures, which causes atherothrombosis resulting in partial (incomplete) occlusion of the coronary artery. NSTE-ACS results in one of the following diagnoses:
- Non ST Elevation Myocardial Infarction (NSTEMI, non-STEMI), if troponin levels are above the upper threshold.
- Unstable angina pectoris (UA) if troponin levels are below the threshold (i.e normal).
- STE-ACS (ST Elevation Acute Coronary Syndrome): STE-ACS occurs when plaque rupture, and the ensuing atherothrombosis, causes a complete occlusion of the coronary artery. Ischemia will extend from the endocardium to the epicardium in the affected myocardial region, which results in ST elevations on the ECG. Virtually all patients with STE-ACS exhibit elevated troponin levels, and are thereby diagnosed as ST elevation myocardial infarction (STEMI).
Chronic Coronary Syndromes (CCS)
Coronary artery disease is a progressive but dynamic disease. The majority of individuals in high-income countries have some degree of coronary atherosclerosis. Risk factors for atherosclerosis (e.g smoking, hypertension, diabetes, hyperlipidemia [particularly high LDL cholesterol], etc) accelerate the atherosclerotic process and increase the number and size of atherosclerotic plaques.
Typically, the first manifestation of coronary artery disease is stable angina, defined by exercise-related chest pain. Patients with stable angina pectoris may develop acute coronary events (acute myocardial infarction, unstable angina) at any time during the disease course. Some patients may experience an acute coronary syndrome as the first manifestation of their coronary artery disease. Moreover, patients who have experienced acute coronary events may, after management of the acute event, be either free from symptoms or continue to experience angina pectoris and other symptoms of ischemia. Thus, coronary artery disease is a nuanced and dynamic condition, which the new guidelines reflect by introducing the concept of chronic coronary syndromes (CCS). The following six categories are included in the CCS spectrum:
- Patients with suspected coronary heart disease with stable angina (chest pain) and/or dyspnea.
- Patients with suspected coronary heart disease and new-onset heart failure or left ventricular dysfunction.
- Patients with stabilized symptoms <12 months after acute coronary syndrome or revascularization.
- Patients with stabilized symptoms >12 months after acute coronary syndrome or revascularization.
- Patients with angina pectoris and suspected vasospasm or microvascular disease.
- Asymptomatic patients in whom coronary heart disease is detected during screening.
These six categories all represent the chronic (non-acute) phases of coronary artery disease.
The natural course in coronary artery disease
Coronary artery disease is caused by atherosclerotic lesions (plaques) in the coronary arteries. Atherosclerotic plaques develop over the course of several decades. LDL cholesterol is fundamental to the initiation and progression of atherosclerosis. Macrophages, T cells and B cells are also key players in the formation of atherosclerotic plaques. LDL cholesterol and immune cells accumulate in the intima and establish a chronic inflammatory process. The diameter of the artery diminishes gradually as the plaque grows. Risk factors of atherosclerosis (e.g smoking, hypertension, diabetes, heredity, etc) accelerate the atherosclerotic process (Libby et al).
As the atherosclerotic plaque grows, blood flow through the stenosis becomes turbulent. This stimulates the endothelium to produce nitric oxide (NO), which causes compensatory vasodilation. Such vasodilation is initially effective; the artery lumen may appear completely normal on coronary angiography. However, in advanced stages of atherosclerosis, this compensatory mechanism fails and the lumen is reduced.
Atherosclerotic plaques exist and grow for several decades before causing clinically overt coronary artery disease. Modern anatomical diagnostic tests (discussed below) can visualize and quantify coronary atherosclerosis long before symptoms appear.
The purpose of early diagnosis and treatment is to slow, inhibit, or reverse the atherosclerotic process. Slowing and inhibition of the atherosclerotic process are considered clinically feasible in the majority of patients (although with difficulties in patients with familial hypercholesterolemia). Moreover, an increasing number of studies show that reversal of the atherosclerotic process may be possible by means of intensive treatment (high dose statins, ezetimibe, PCSK9 inhibitors, and intensive lifestyle changes; Fisher et al).
Unless plaque rupture occurs, coronary artery disease is asymptomatic until the plaque prevents adequate blood flow across the stenosis. The majority of all stenoses that obstruct <50% of the diameter do not produce any symptoms. Stenoses obstructing 50–90% of the lumen may cause symptomatic ischemia. Stenoses obstructing >90% of the lumen mostly cause symptomatic ischemia (Knuuti et al, Tonino et al). Thus, there is substantial redundancy in the coronary perfusion.
In the early stages of coronary artery disease, ischemia occurs only during exercise. Myocardial oxygen demand increases during exercise but the stenosis prevents the necessary increase in oxygen delivery (i.e coronary perfusion). As atherosclerosis progresses, the stenosis becomes larger, such that lower levels of exercise are required to provoke angina.
At any time during the course of the disease, an acute coronary syndrome may occur. This is explained by the vulnerability of atherosclerotic plaques. Plaques may rupture completely, or erosion may occur on the cap. Either scenario results in vascular collagen being exposed to von Willebrand factor (vWF) in the blood, which triggers thrombocyte activation, aggregation and atherothrombosis. The thrombus may cause a complete or partial (incomplete) occlusion of the artery. Complete occlusions typically cause STEMI, whereas partial occlusions lead to NSTEMI or UA.
Plaque rupture or erosion can occur in small or large plaques, which means that an acute coronary syndrome may occur both early or late in the disease course. This explains why acute coronary syndromes may be the initial clinical manifestation of coronary heart disease, including in young people (Arbab-Zadeh et al).
Definition of stable and unstable angina
Stable coronary artery disease (angina pectoris)
In classical angina pectoris, the pain is typically localized near the sternum. Pain may radiate to the back, neck, jaw, or arms. Inferior wall ischemia/infarction may cause pain located primarily in the epigastrium.
The pain is typically described as a pressure, cramp, tightness, heaviness or discomfort in the chest. A burning sensation is less common, and may be confused with gastroesophageal reflux. Pain or discomfort caused by myocardial ischemia has no correlation to respiratory movements, thoracic or body movements. Instructing the patient to take deep breaths, hold the breath, and perform thoracic movements (rotation, extension, flexion) can elucidate this. Cold sweats, fatigue and anxiety are common during myocardial ischemia and infarction.
Dyspnea is also common during angina, especially among the elderly, women and individuals with diabetes. Because dyspnea may be the only manifestation of myocardial ischemia, it is considered an anginal equivalent.
The duration of chest pain is less than 10 minutes in patients with stable angina pectoris, with most episodes lasting one or a few minutes (provided that the activity provoking the pain is stopped). Chest pain lasting a few seconds is a common complaint, both in the primary care setting and in the emergency room, and is rarely caused by ischemia. Ischemic chest pain lasting >10 minutes is likely to be due to an acute coronary syndrome. Patients with stable coronary artery disease should therefore be instructed to seek medical attention if chest pain lasts 10 minutes or longer, particularly if administration of nitrates do not relieve the pain.
Nitrates induce arterial and venous vasodilation, which reduces left ventricular preload and afterload, and thereby reduces myocardial workload. Nitrates relieve angina within one or two minutes. Multiple doses (discussed below) may be necessary, depending on the severity of ischemia. Because nitrates may have a placebo effect it is not possible to rule-in myocardial ischemia based on the response to nitrates. However, the probability of ischemia as the underlying cause increases if nitrates alleviate the symptoms.
Angina pectoris is aggravated by physical exertion, cold weather, heavy meals and in the morning hours. The level of physical exertion causing angina is called anginal threshold. This threshold may vary on a day to day basis. Warm-up angina is an unusual phenomenon, whereby exercise-induced ischaemia is reduced or abolished on a second effort following the first effort after a brief pause (Williams et al). Walk-through angina, a rare phenomenon, is defined as the emergence of angina during the first stages of exercise with disappearance of chest pain at higher workloads, despite a greater rate-pressure product (Gavazzi et al).
In stable angina, symptoms are stable over time (no worsening in the last month) and no symptoms are present at rest.
The ECG in stable coronary artery disease
The ECG shows no signs of acute ischemia at rest, unless there is ongoing myocardial ischemia, which may be symptomatic or asymptomatic.
Recommended chapter: The ECG in myocardial ischemia.
Troponin levels in stable coronary artery disease
Troponin levels are normal in the majority of patients with stable angina pectoris. It should be noted, however, that up to 30% of patients with stable coronary artery disease may exhibit elevated troponin levels (Everett et al), which is associated with an increased risk of cardiovascular death. These patients display steadily elevated troponin levels, as compared to the dynamic changes observed during acute myocardial infarction.
Stable angina pectoris is classified according to criteria presented in Table 1. This classification is based solely on symptoms and is used to assess the probability that symptoms are explained by myocardial ischemia (angina).
Table 1. Classification of Angina Pectoris.
| Classification | Definition |
|---|---|
| Typical angina pectoris | Typical angina meets all three of the following criteria: 1) Pressure discomfort anteriorly on the thorax, in the neck, jaw, shoulders or arm. 2) Angina in physical exertion 3) The pain is relieved by rest or with the help of nitro preparations |
| Atypical angina pectoris | Atypical angina meets two of three above criteria. |
| Non-anginal chest pain or discomfort | Non-anginous chest pain meets one or none of the criteria. |
Definition of unstable angina pectoris (UA)
Unstable angina pectoris is an acute coronary syndrome and is present if any of the following occurs:
- Angina at rest.
- New onset angina (last 2 months) of CSS class II to III (Table 2).
- Crescendo angina (angina that has worsened significantly in recent days or weeks).
Table 2. Canadian Cardiovascular Society Classification of Angina Pectoris
| Class | Severity |
|---|---|
| Class I | Angina only during strenuous or prolonged physical activity. |
| Class II | Slight limitation, with angina only during vigorous physical activity. |
| Class III | Symptoms with everyday living activities, ie, moderate limitation. |
| Class IV | Inability to perform any activity without angina or angina at rest, ie, severe limitation. |
Evaluation of suspected chronic coronary artery disease
Sensitivity and specificity for diagnostic tests
A diagnostic test is defined in this context as an investigation that can diagnose or exclude coronary artery disease. All diagnostic tests can be evaluated using the following parameters:
- Sensitivity: the proportion (%) of positives (i.e who have coronary artery disease) who are correctly identified.
- Specificity: the proportion (%) of negatives (i.e who do not have coronary artery disease) who are correctly identified.
- PPV (positive predictive value): The probability (%) that the patient has the disease if the test is positive.
- NPV (negative predictive value): The probability (%) that the patient does not have the disease if the test is negative.
- PTP (pre-test probability): the probability that the patient has the disease (coronary artery disease), based on the history and clinical findings.
Pre-test probability is related to Bayes’ theorem, which states that the probability of an event is dependent on the probability of a prior event. In this scenario, the probability of a patient having coronary artery disease depend on age, cholesterol levels, smoking status, blood pressure, type of symptoms, etc. The clinical utility of Baye’s theorem cannot be overstated. It is fundamental to assess pre-test probability before conducting any investigations.
Traditionally, exercise ECG has been the first choice for evaluating patients with suspected coronary artery disease. This has been revised in the new guidelines (Knuuti et al). Exercise ECG is no longer the recommended initial test. Exercise ECG is nowadays recommended only to evaluate the following:
- Assessment of exercise capacity.
- Assessing the risk of developing arrhythmias during exercise.
- Evaluating the effect of treatments (e.g anti-anginal medications) and interventions (e.g CABG, PCI).
- Assessing anginal threshold.
- Evaluating blood pressure reaction.
Table 3 presents the sensitivity and specificity of various diagnostic test available.
Table 3: Test Sensitivity and Specificity for Coronary Artery Disease
| Modality | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Exercise stress testing (exercise ECG) | 40-50% | 85 -90% |
| Stress echocardiography | 80-85% | 80-88% |
| Stress SPECT | 73-92% | 63-87% |
| Stress echocardiography with dobutamine | 79-83% | 82-86% |
| Stress MRI with dobutamine | 72-79% | 81-91% |
| Stress echocardiography with vasodilator | 90-91% | 75-84% |
| Stress SPECT with vasodilator | 67-94% | 61-85% |
| CTA coronary artery | 95-99% | 64-83% |
| Stress PET with vasodilator | 91-97% | 74-91% |
Evaluation of suspected coronary artery disease with angina pectoris and/or dyspnea
Figure 1 summarizes the investigation and management of patients with suspected coronary artery disease. The procedure consists of six steps, which are discussed here below.

Step 1. History and Clinical Examination
Symptoms and medical history are fundamental in investigating suspected coronary heart disease. The chest pain is classified into one of the following three categories: typical angina, atypical angina or non-anginal chest pain (Table 1).
If symptoms are suggestive of an ongoing acute coronary syndrome (ACS), then it should be determined whether it is STEMI or NSTEMI/UA, with appropriate measures executed. It is crucial to always rule out an ongoing acute coronary syndrome in patients that are under evaluation.
Risk factors for coronary artery disease must be scrutinized meticulously. These include hyperlipidemia (dyslipidemia, high LDL cholesterol), diabetes (type 1 diabetes, type 2 diabetes), smoking, hypertension, heredity, low intake of fruits and vegetables, physical inactivity, male sex and advanced age. The probability of coronary artery disease increases exponentially with the number of risk factors present (Yusuf et al, INTERHEART Study).
Step 2. Assess prognosis, quality of life, comorbidities
Investigative efforts depend on the patient’s preferences and health status. Patients who prefer to be investigated and who have a significant quality of life, as well as life-expectancy, should be investigated. Patients with severe comorbidities, low quality of life and/or low life-expectancy should not undergo further investigation. These patients can be diagnosed based on findings in Step 1 and subsequently offered OMT (optical medical therapy).
Step 3. Blood tests, ECG, echocardiography, MRI & chest X-ray
ECG
All patients should be examined with a 12-lead resting ECG. The following principles apply with regards to ECG changes:
- The ECG shows ST deviation during ongoing ischemia:
- ST depression and ST elevation indicate ongoing ischemia.
- The ECG shows T-wave inversion (negative T waves) after an ischemic episode (post-ischemic T-wave inversions).
- The ECG shows pathological Q-waves or R-wave progression after manifestation of myocardial infarction.
If a patient experiences chest pain when a 12-lead ECG is recorded, and the ECG does not display ST deviations, then it is very unlikely that the chest pain is due to ischemia. Patients with ongoing ischemic chest pain virtually always exhibit ST deviations on the ECG.
Read more: The ischemic cascade.
The following ECG changes correlate with, but are not specific to, coronary heart disease:
- Left bundle branch block (LBBB) is common in individuals with coronary artery disease.
- AV block I, AV block II, AV block III are also common in individuals with coronary artery disease.
- Atrial fibrillation is also associated with coronary artery disease.
Blood tests
- Glucose, HbA1c, BMI, waist hip ratio.
- Blood lipids include total cholesterol, LDL cholesterol, triglycerides, HDL cholesterol and non-HDL cholesterol. Fasting samples are only necessary in cases with extreme hypercholesterolemia, or if triglycerides are very high (Ference et al).
- In case of suspicion of hyperthyroidism or hypothyroidism: TSH, T4, T3.
- Sodium (Na+), potassium (K+), creatinine, calculation of estimated GFR (eGFR).
- In case of suspicion of acute coronary syndrome: troponin T or troponin I.
- In case of suspicion of heart failure: NT-proBNP or BNP.
Echocardiography
Echocardiography should be done routinely in patients with coronary artery disease. Measurement of ejection fraction, systolic function, dimensions, valvular function, diastolic function, etc, may impact treatments and investigations.
Cardiac magnetic resonance imaging (cardiac MRI)
Magnetic resonance imaging provides detailed and comprehensive assessments of myocardial anatomy, function and scarring, as well as valvular function. Myocardial scarring (infarction) is visualized using gadolinium contrast.
Chest X-ray
Chest X-ray is only indicated if there is a suspicion of congestive heart failure.
Step 4. Calculate PTP and clinical probability of coronary artery disease
Pre-test probability (PTP) is the likelihood that the patient has coronary artery disease, based on history and clinical data. The likelihood of coronary artery disease is a function of disease prevalence and patient characteristics.
If the patient represents a population with a high prevalence of coronary heart disease and exhibits all symptoms of the disease, then PTP is very high. In that scenario, the usefulness of diagnostic tests decreases because they will almost certainly only confirm an already probable diagnosis. The opposite is also true; if the disease is rare and the patient presents no symptoms consistent with the disease, then an examination is unlikely to reveal anything useful. In general, diagnostic tests are most useful when used in patients with an intermediary likelihood of disease.
- If the probability of coronary heart disease is low and the examination is negative, then coronary heart disease can be excluded.
- If the probability of coronary heart disease is high and the examination is positive, then coronary heart disease can be confirmed.
Pre-test probability of coronary heart disease is estimated based on sex, age and symptoms (Figure 2).
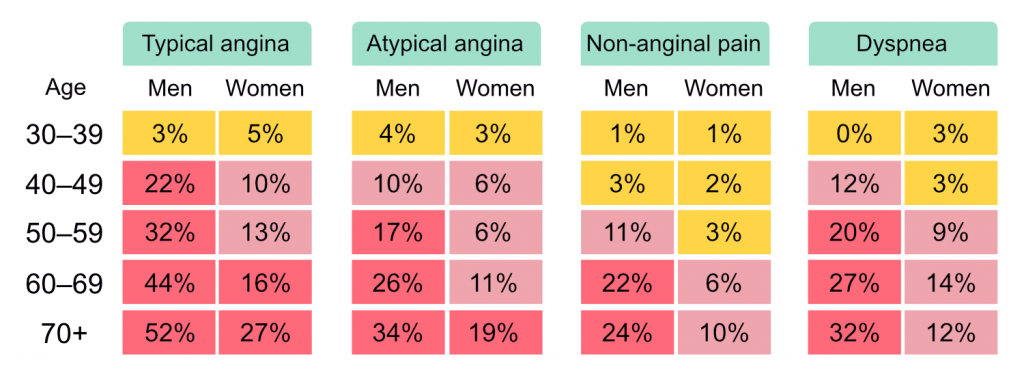
If PTP is <5% then coronary artery disease is unlikely. This should imply that other diagnoses are more likely, and additional investigations for coronary artery disease should only be done in special circumstances. The usefulness of non-invasive tests is greatest if PTP is >15%.
If PTP is 5 to 15%, the following parameters should be taken into account for assessing the clinical likelihood of coronary heart disease:
- Risk factors
- Medical history and status
- ECG findings
- Echocardiographic findings.
The clinical probability of coronary artery disease increases with the number of factors that are consistent with coronary artery disease. Thus, the clinical probability of coronary heart disease is the sum of PTP and the above parameters (risk factors, history, status, resting ECG, echocardiography).
Coronary calcium score can be considered when assessing clinical probability. Note, however, that some atherosclerotic plaques have a low calcium concentration, despite high grade stenosis, which is why calcium score can not be used to exclude coronary heart disease.
Step 5. Selecting the appropriate diagnostic tests
There are three strategies for diagnosing coronary artery disease using imaging and functional tests.
- Functional non-invasive examinations
- Exercise ECG → assessment of ischemic ECG changes.
- Stress echocardiography → assessment of wall motion abnormalities.
- Stress MRI → assessment of wall motion abnormalities.
- Contrast (gadolinium) MRI → assessment of perfusion abnormalities.
- SPECT → assessment of perfusion abnormalities.
- PET → assessment of perfusion abnormalities.
- Anatomical non-invasive examinations
- CT angiography of coronary arteries
- Invasive coronary angiography (ICA)
- Possibility is available for assessment of stenosis hemodynamic effects (with FFR [fractional flow reserve]).
Stress can be induced by exercise or by vasodilation of coronary arteries.
Anatomical vs. functional tests
Anatomical non-invasive examinations visualize the coronary artery lumen and wall. This allows for direct visualization of atherosclerotic plaques and quantification of any stenosis. The stenosis is quantified by measuring the percentage of the lumen obstructed. CT angiography of coronary arteries has very high sensitivity to atherosclerotic plaques. This method detects both large and small stenoses, but cannot assess whether they are hemodynamically significant. In general, obstruction <50% of the diameter causes no symptoms (but the patient still has atherosclerosis and is therefore at risk of acute coronary events). Obstruction in the range 50–90% of the diameter may be hemodynamically significant (i.e cause angina pectoris and ischemia). Plaques obstructing >90% are very likely to be clinically significant. Nevertheless, a functional test is necessary to determine the hemodynamic significance of any plaque.
Functional tests are excellent for revealing clinically significant stenoses. However, functional tests do not detect subclinical atherosclerosis. CT angiography of coronary arteries detect all levels of atherosclerosis.
Recommendations for selection of diagnostic tests
CT angiography of the coronary arteries is the preferred method if the clinical probability is in the lower range. Note that this study is not suitable for patients with ongoing atrial fibrillation (or other arrhythmias causing irregular rhythm) or high coronary calcium score since the image quality is hampered in these scenarios.
Non-invasive functional examination is preferred if the clinical probability is in the higher range, or if the patient has known coronary artery disease. A positive non-invasive functional test indicates that a clinically significant stenosis exists.
Invasive angiography is done if non-invasive investigations have been inconclusive and suspicion remains. Invasive angiography can also be considered as an initial test if the clinical probability is very high, the short-term risk of cardiovascular events is high and/or if pronounced symptoms persist despite optimal medical therapy.
Step 6. Assess prognosis and risk of cardiovascular event
All patients should receive optimal medical therapy (OMT). During the course of the disease, the risk of myocardial infarction and cardiovascular death should be reassessed, and the indication for invasive angiography should be reassessed continuously. The purpose of angiography is to assess the need for revascularization (discussed below).
Treatment of coronary artery disease
Treatment goals for patients with coronary artery disease include the following:
- Improve prognosis (i.e prolong survival).
- Reduce symptoms.
- Improve functional capacity.
- Improve quality of life.
Large clinical trials typically measure the effect of an intervention on the risk of incident (i.e new) or recurring cardiovascular events, development of complications (e.g heart failure), and mortality. Such outcome measures are referred to as hard endpoints. Very few drugs have effects on hard endpoints, particularly mortality. The most effective drugs, as defined by the number needed to treat, in patients with stable coronary artery disease are arguably aspirin (acetylsalicylic acid) and statins (Collins et al). Other commonly used drugs, e.g angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARB), beta-blockers, calcium channel blockers, etc have little or no significant effect on hard endpoints. The effect of ACE inhibitors, ARBs and beta-blockers appear to be restricted to patients with hypertension, left ventricular dysfunction and/or heart failure.
Multidisciplinary management
Management of patients with coronary artery disease (i.e chronic coronary syndromes) requires a multidisciplinary team led by a physician and a nurse. Most patients can be managed in the primary care setting unless symptoms or disease progression are ominous. The multidisciplinary team includes physicians, nurses, physiotherapists, dietitians, psychologists, therapists, and others. Clinical trials demonstrate that multidisciplinary management increases well-being, adherence to medical therapy, multifactorial risk factor control and PROM (patient reported outcome measures).
It should be noted that even in health care systems with virtually free access to medications, patients with acute myocardial infarction typically use 50% of their prescribed doses of statins and aspirin (Hero et al). Adherence to all medications must be continuously monitored and promoted.
A physician is responsible for instigating medical therapies and assessing whether known or suspected coexisting conditions require additional investigations and treatments. All medical therapies should be followed up in order to assess side effects, titrate doses, and evaluate whether additional therapy is warranted.
Smoking cessation
Smoking is second only to dyslipidemia the strongest risk factor for coronary artery disease and acute myocardial infarction. Smoking cessation should be promoted by means of counseling and pharmacological therapy. All forms of systematic counseling are effective and increase the likelihood of smoking cessation. Nicotine replacement, bupropion and varenicline are safe and more effective than placebo (Mills et al).
E-cigarettes may be more effective than nicotine-replacement, although the long-term effects of e-cigarettes are unknown and there are reports of harmful effects (Hajek et al)
Diet and coronary artery disease
Patients with coronary heart disease should, according to the European Society for Cardiology and the American Heart Association, increase the intake of polyunsaturated fat, fibre, legumes, nuts, vegetables and fruit. Saturated fats, red meat, sugary beverages, and carbohydrate-rich food should be avoided.
It should be noted, however, that several large clinical trials have indicated that a low carbohydrate diet (i.e high fat diet) may have more beneficial effects on blood lipids, blood pressure and inflammatory markers (Shai et al, NEJM). There are also studies suggesting that saturated fats do not increase the risk of coronary artery disease (Dehghan et al, The Lancet), and the long-standing notion that fish oil (omega 3) protects against coronary artery disease lacks evidence (Aung et al, JAMA).
There is also evidence that a Mediterranean diet may be beneficial in reducing the risk of cardiovascular events (Estruch et al, NEJM).
Despite the inconsistencies in dietary data, it is reasonable to recommend increased intake of fruit, nuts, vegetables, legumes and unsaturated fats. Fibre and white meat should be preferred over carobhydrates with high glycemic index and red meat (although the latter is also questioned by data).
It is fundamental to distinguish dietary lipids from blood lipids. The correlation between dietary lipids (fat) and blood lipids ( including LDL cholesterol) is generally weak. Patients with very high fat intake (including saturated fats) may have low LDL cholesterol, and vice versa (Mente et al, The Lancet).
Alcohol
Consumption of 1-2 standard drinks per day is not associated with an increased risk of acute myocardial infarction. The lowest overall mortality is observed at zero intake of alcohol (The GBD Study, The Lancet).
Overweight and obesity
Overweight (defined as BMI 25–30 kg/m) and obesity (defined as BMI >30 kg/m2) cause dyslipidemia (hyperlipidemia), hypertension, dysglycemia (hypergylcemia), diabetes, coronary artery disease, peripheral artery disease, acute myocardial infarction, heart failure, specific cancers and premature death (Heymsfield, NEJM, 2017). The risk of these complications increases with BMI.
BMI is, however, inferior to waist hip ratio (WHR) with regards to predicting cardiovascular events and diabetes. This is explained by the fact waist circumference correlates better with central obesity, which is causally linked to the metabolic syndrome, diabetes, cardiovascular risk factors and events.
Weight loss is recommended in patients with BMI >25 kg/m2. Recommended BMI for patients with coronary artery disease is 20–25 kg/m2. Recommendations for waist circumference are as follows:
- Females: ≤80 cm
- Males, Caucasian or African American: ≤94 cm
- Males, South-Asian: ≤90 cm
South-Asians are at higher risk of diabetes at every BMI level (Ramachandran et al, The Lancet).
The most effective method for weight loss is reducing calorie intake. Low-calorie diets result in immediate weight loss but are difficult to maintain. Indeed, any diet resulting in calorie reduction will cause weight loss, including fad diets (e.g low carbohydrate diet, Atkin’s diet, etc). There is no evidence to unequivocally prove that any specific diet has metabolic advantages. A recent study compared gastric bypass and calorie reduction and reported that the method of weight loss was not of significance (Johannis, NEJM, 2020).
Gastric bypass should be considered in patients with severe obesity.
Glucagon-like peptide-1 receptor agonists, also known as GLP-1 receptor agonists or incretin mimetics, are agonists of the GLP-1 receptor. They are indicated to treat type 2 diabetes as well as obesity. GLP-1 receptor agonists result in 4 kg mean weight loss (by reducing appetite), while also reducing the risk of cardiovascular events. Currently available GLP-1 receptor agonists:
- Exenatide (Byetta, Bydureon), approved in 2005/2012.
- Liraglutide (Victoza, Saxenda), approved 2010.
- Lixisenatide (Lyxumia in Europe, Adlyxin in the United States).
- Albiglutide (Tanzeum, approved in 2014.
- Dulaglutide (Trulicity, approved in 2014.
- Semaglutide (Ozempic, Rybelsus).
Diabetes
Coronary artery disease is the leading cause of death in people with diabetes. Atherosclerosis is accelerated in people with type 1 diabetes and type 2 diabetes (Rawshani et al, The Lancet). Guidelines recommend starting statin therapy at age 40 in all people with diabetes (The Heart Protection Study, The Lancet). With regards to glycemia, most studies have demonstrated that glycated hemoglobin A1c (HbA1c, A1c) is the best predictor of macrovascular disease (acute myocardial infarction, coronary artery disease, stroke, peripheral artery disease), heart failure, and microvascular disease (retinopathy, neuropathy, nephropathy). The existence of microvascular disease is a strong predictor of macrovascular disease.
Multifactorial risk factor control is key to reduce the risk of acute myocardial infarction and heart failure in people with diabetes (Rawshani et al, NEJM). Details regarding the management of hyperglycemia are discussed in American Diabetes Association’s Standards of Care, and the European Association for the Study of Diabetes Guidelines:
Beta-blockers
Beta-blockers bind to beta-adrenoceptors and block the effect of norepinephrine and epinephrine. Beta-blockers thereby inhibit sympathetic activity. Non-selective beta-blockers block both beta-1 (β1) and beta-2 (β2) adrenoceptors. Selective beta-blockers are preferred in patients with coronary artery disease, as well as heart failure, and are relatively selective for cardiac β1 adrenoceptors.
By inhibiting sympathetic activity, beta-blockers reduce heart rate and myocardial contractility (i.e beta-blockers have negative inotropic effect). Reduction in heart rate and contractile force results in reduced myocardial workload and oxygen consumption. Reduction in heart rate also leads to prolongation of diastole, which increases the time period for myocardial perfusion (coronary perfusion occurs during diastole).
Beta-blockers alleviate angina pectoris, lower blood pressure, improve exercise capacity, and reduce ischemic episodes. All patients with coronary heart disease should be treated with beta-blockers, despite the fact that several randomized trials have failed to demonstrate that beta-blockers improve survival in patients with coronary artery disease unless they have experienced an acute myocardial infarction. All available beta-blockers are equally effective.
Resting heart rate should be 55 to 60 bpm with the use of beta-blockers.
Table 4: Beta-blockers.
| Category | Agents |
|---|---|
| Non-selective beta-blockers | Propranolol Bucindolol (has α1-blocking activity) Carteolol Carvedilol (has α1-blocking activity) Labetalol (has α1-blocking activity) Nadolol Oxprenolol (has sympathomimetic activity) Penbutolol (has sympathomimetic activity) Pindolol (has sympathomimetic activity) Sotalol (atypical beta blocker) Timolol |
| β1 selective beta-blockers | Acebutolol (has sympathomimetic activity) Atenolol Betaxolol Bisoprolol Celiprolol (has sympathomimetic activity) Metoprolol Nebivolol Esmolol Nebivolol (also β1 agonist) |
| β2 selective beta-blockers | Butaxamine |
Beta-blocker therapy is titrated slowly. A starting dose of metoprolol 25 mg once a day is safe and can be doubled every two weeks until maximally tolerated dose, or maximum dose (200 mg), is achieved. Beta-blockers are well tolerated and few patients have clinically significant side effects that require discontinuation of therapy. The indication for beta-blockers is relatively strong and termination is only done after careful consideration.
If beta-blockers do not provide sufficient symptom relief (or cause adverse side effects), calcium channel blockers (diltiazem, verapamil [amlodipine in patients with heart failure]) may be tested.
Most patients with chronic obstructive pulmonary disease (COPD) tolerate beta-blockers, despite the theoretical risk for exacerbation of airway obstruction. Non-selective beta-blockers should be avoided in patients with COPD.
The indication for beta-blocker therapy is very strong in patients with heart failure, such that discontinuation should only be considered if absolutely necessary.
Discontinuation of beta-blockers is done gradually over a period of 30 days.
Side effects of beta-blockers: AV-blocks, depression, impotence, nightmares, bradycardia, fatigue, reduced exercise capacity, bronchospasm. Masking of hypoglycemia is frequently mentioned as a side effect in the literature, although it is very rare in clinical practice; diabetes is not a contraindication to beta-blockers.
Calcium channel blockers (CCB)
Calcium channel blockers reduce heart rate and lower blood pressure, thereby reducing angina and ischemia. Randomized clinical trials have not demonstrated a survival benefit from calcium channel blockers (Knuuti et al). The anti-anginal effect of calcium-channel blockers is on a par with beta-blockers.
Non-dihydropyridines include verapamil and diltiazem. These agents lower heart rate, lower blood pressure and prevent coronary vasospasm. Verapamil is used frequently in patients with coronary artery disease.
Table 5. Calcium channel blockers.
| Verapamil | Diltiazem | Amlodipine, Felodipine, Isradipine, Nicardipine, Nifedipine, Nimodipine, Nitrendipine | |
|---|---|---|---|
| CLASS | Non-dihydropyridines | Non-dihydropyridines | Dihydropyridines |
| SELECTIVITY | Cardiac calcium channels | Cardiac calcium channels and vascular L-type calcium channels. | Vascular L-type calcium channels |
| NEGATIVE INOTROPIC EFFECT | Yes. Should be avoided in heart failure. | Yes. Should be avoided in heart failure. | No. Can be used in heart failure. |
| REDUCTION OF HEART RATE | Yes | Yes | No |
| ANTI-ANGINAL EFFECT | Yes, pronounced. | Yes, pronounced. | Yes, less than verapamil and diltiazem. |
| BLOOD PRESSURE LOWERING EFFECT | Small | Small | Pronounced |
| VASOSPASTIC EFFECT | Reduces vasospasm. | Reduces vasospasm. | Reduces vasospasm. |
| SIDE EFFECTS | Bradycardia, AV-blocks, negative inotropic effect. Should not be combined with beta-blockers due to risk of AV-block. | Cardiac side effects less pronounced as compared with verapamil. Bradycardia, AV-blocks, negative inotropic effect. Should not be combined with beta-blockers due to risk of AV-block. | Flushing, headache, excessive hypotension, ankle edema, reflex tachycardia. Amlodipine may be combined with beta-blockers. |
Ivabradine
Blocks If (cardiac funny channels) in the sinoatrial node, which reduces heart rate in patients with sinus rhythm, and thereby reduces angina and ischemia. Ivabradine does not reduce the risk of cardiovascular events in patients with coronary artery disease (Fox et al).
If channels establish the pacemaker current that causes spontaneous depolarizations in sinoatrial cells. Ivabradine reduces heart rate without affecting blood pressure or contractility, and may therefore be used in patients with heart failure. The anti-anginal effect of ivabradine is due to its slowing of the heart rate. Ivabradine is typically indicated if resting heart rate is >70 beats per minute.
Brand names: Corlanor, Procoralan.
Ivabradine is recommended to relieve angina as a second line therapy.
Nitrates
Nitrates primarily induce venous vasodilation by increasing endothelial production of nitric oxide (NO). Venous dilation results in reduced venous return, reduction in cardiac preload and thereby reduced myocardial workload. Short-acting nitrates provide immediate relief of angina. Long-acting nitrates relieve angina within 5 minutes and may last for several hours. Nitrates do not affect mortality or morbidity. All patients with coronary artery disease should be provided with short-acting nitrates.
Severe aortic stenosis and hypertrophic obstructive cardiomyopathy are contraindications to nitrates.
Commonly used nitrates
- Nitroglycerin
- Sublingual tablet – 0.3 to 0.6 mg, up to 1.5 mg as needed a day
- Transdermal patch – 0.2 – 0.8 mg/h, one patch a day (remove at night for 12h)
- Capsule – 5 – 6.5 mg, 3 to 4 times a day
- Spray – 0.4 to 0.8 mg, 1 to 3 times a day; max 3 actuations in 15 minutes
- Intravenous – 10 to 120 μg/min
- Isosorbide dinitrate
- Tablet – 10 to 40 mg 3 times a day
- Sublingual tablet – 2.5 to 10 mg
- Spray – 1.25 mg per dose
- Isosorbide mononitrate
- Tablet – 20 mg twice daily
- Tablet, sustained release – 30 to 120 daily; max daily dose 240 mg daily
Administration of nitrates during acute chest pain
- Nitrates are administered in a sitting position.
- Dose: 0.4 mg nitroglycerin spray or 0.3-0.6 mg sublingual tablet.
- Dose is repeated every 5 minutes as necessary, until maximum dose 1.2 mg.
- If angina persists after 15 minutes, an acute coronary syndrome should be suspected.
Long-acting nitrates may be considered as angina prophylaxis if beta-blockers and calcium channel blockers are insufficient. Long-acting nitrates exacerbate reflex tachycardia and must therefore not be introduced before beta-blockers have been maximally titrated. Long-acting nitrates are introduced gradually to avoid side effects.
Side effects of nitrates: hypotension, headache, flushing, syncope, reflex tachycardia.
Contraindications to nitrates
- Allergy to nitrates
- Concomitant use of phosphodiesterase (PDE) inhibitors such as tadalafil and sildenafil.
- Right ventricular infarction
- Hypertrophic cardiomyopathy
- Severe aortic stenosis.
Nicorandil
Nicorandil provides anti-anginal effects and may be used as second-line therapy for refractory angina.
Ranolazine
Ranolazine provides anti-anginal effects and may be used as second-line therapy for refractory angina.
Side effects: QT prolongation, dizziness, nausea, constipation.
Trimetazidine
Trimetazidine also provides anti-anginal effects and may be used as second-line therapy for refractory angina.
Platelet inhibition (antiplatelet drugs)
Platelet inhibition is the most effective means of reducing the risk of unstable angina, NSTEMI, STEMI, stent thrombosis, re-infarction, and cardiovascular death in patients with coronary artery disease. Platelet inhibition is superior to anticoagulants, including NOACs, in terms of preventing atherothrombosis. Several drug classes have been developed, all of which target key elements of platelet activation and aggregation. Figure 3 demonstrates the cellular and molecular processes resulting in atherothrombosis. Figure 4 depicts the cellular targets exploited by antiplatelet drugs.

The purpose of antiplatelet drugs is to inhibit platelet activation and aggregation (adhesion) in the setting of plaque rupture or erosion. A ruptured or eroded plaque exposes vascular collagen to von Willebrand factor in the blood. Binding of von Willebrand factor to collagen enables platelets to attach to the former and trigger cellular processes leading to platelet aggregation and activation of coagulation factors.
Platelet activation and adhesion depend on several cellular mechanisms that are targeted by antiplatelet drugs. All currently available drugs induce a constant state of platelet inhibition, which results in an increased risk of fatal and non-fatal bleeding events. It is crucial to carefully balance bleeding risk with thrombotic risk when making treatment decisions. This is particularly important in the following patients:
- Elderly individuals.
- Individuals with chronic kidney disease (CKD).
- Individuals who undergo PCI (primary or elective), since these patients require combination therapy with two antiplatelet drugs for up to 12 months after the procedure. Combination therapy with two antiplatelet drugs is referred to as DAPT (dual antiplatelet therapy).
- Patients who are treated with OAC (oral anticoagulants), e.g atrial fibrillation, pulmonary embolism, mechanical valves, etc.
Types of platelet inhibitors
- NSAID (non-steroidal anti-inflammatory drugs): Only aspirin (acetylsalicylic acid) is licensed for the treatment of coronary artery disease.
- Oral P2Y12 inhibitors: clopidogrel, prasugrel, ticagrelor.
- Intravenous P2Y12 inhibitors: cangrelor.
- Glycoprotein IIb/IIIa (GP IIb/IIIa) inhibitors: abciximab, eptifibatide, tirofiban, roxifiban, and orbofiban are used during PCI.

Table 5: Antiplatelet drugs
| Class | Agent | Brand names | Indication in CCS |
|---|---|---|---|
| NSAID | Acetylsalicylic acid | Aspirin | All patients with CCS should receive aspirin. |
| P2Y12 Inhibitors | Ticagrelor | Brilinta, Brilique | Yes |
| Cangrelor | Kengreal | During PCI | |
| Prasugrel | Effient | Yes | |
| Clopidogrel | Plavix | Yes | |
| GP IIb/IIIA inhibitors | Tirofiban | Aggrastat | During PCI |
| Abciximab | ReoPro | During PCI | |
| Eptifibatide | Integrilin | During PCI | |
| PAR-1 antagonists | Vorapaxar | Zontivity | No |
Aspirin (acetylsalicylic acid)
Recommendation: All patients with coronary heart disease should receive ≥75 mg aspirin once daily. Aspirin is used in DAPT in all patients who tolerate the drug.
Aspirin reduces the production of TXA2 (Thromboxane A2) by inhibiting COX-1 (Cyclooxygenase-1). TXA2 stimulates platelet adhesion. It has been speculated as to whether aspirin may also reduce plaque inflammation and growth.
Several landmark trials have demonstrated that aspirin is very effective in preventing acute myocardial infarction. Aspirin is safe, well tolerated, inexpensive and does not require monitoring of hemostasis. Aspirin is indicated in all patients with chronic and acute coronary syndromes. Aspirin reduces the risk of death and acute myocardial infarction by 33% in patients with angina pectoris (ISIS-2, ISIS-3).
A dose of 75 mg once daily disables approximately 80% of all platelets. Studies show that doses in the range 75 mg to 1500 mg are equally effective in terms of preventing atherothrombosis, but the risk of fatal and non-fatal hemorrhages increases with higher doses.
There are no data to support the use of other NSAIDs (ibuprofen, naproxen, diclofenac, celecoxib, etoricoxib) to manage coronary artery disease. COX-1 selective NSAIDs (celecoxib) may increase the risk of cardiovascular death (Nissen et al, NEJM).
P2Y12 inhibitors
P2Y12 receptors are located on the cell membrane and stimulates platelet aggregation by increasing the expression of glycoprotein IIb/IIIa (GP IIb/IIIa) receptor. GP IIb/IIIa connects platelets via fibrinogen. Inhibition of the P2Y12 receptor results in reduced expression of GP IIb/IIIa.
- Prasugrel: irreversible inhibition of P2Y12. Delivered as a prodrug that must be converted to its active metabolite in the liver.
- Clopidogrel: reversible inhibition of P2Y12. Also delivered as a prodrug that must be converted to its active metabolite in the liver.
- Ticagrelor: reversible inhibition of P2Y12. Ticagrelor has immediate effect.
- Cangrelor: only used during PCI.
Clopidogrel
Clopidogrel 75 mg once daily is equal to aspirin with regards to efficacy and safety. Clinical trials with head-to-head comparison of clopidogrel and aspirin (The CAPRIE Study) demonstrate that the effect of clopidogrel on acute myocardial infarction, ischemic stroke, and death is at least equal to aspirin.
Clopidogrel is converted to its active metabolite by the cytochrome P450 enzyme CYP2C19. Some genetic variants in CYP2C19 lead to reduced conversion to the active metabolite, rendering clopidogrel less effective. Genotyping is possible but not recommended (Knuuti et al, Aradi et al). Omeprazole and esomeprazole inhibits CYP2C19 and thereby reduces the effect of clopidogrel.
Recommendations:
– Patients who have contraindications or allergy to aspirin should receive clopidogrel 75 mg once daily.
– Clopidogrel should not be combined with omeprazole or esomeprazole.
– Clopidogrel may be used in DAPT.
Prasugrel
Prasugrel has primarily been studied in patients undergoing PCI. Prasugrel provides constant, rapid and effective platelet inhibition. Prasugrel is more potent than aspirin and clopidogrel, and reduce the risk of ischemic events during and after PCI, although with increased risk of fatal and non-fatal hemorrhages (Knuuti et al).
Recommendations: In patients undergoing elective PCI, prasugrel is considered if thrombotic risk is high during or after the procedure, or if DAPT with aspirin and clopidogrel is not possible.
Ticagrelor
Recommendations:
– In patients undergoing elective PCI, ticagrelor is considered if thrombotic risk is high (e.g unfavorable stenting results or multivessel disease) or if DAPT with aspirin and clopidogrel is not feasible.
– Ticagrelor may be combined with aspirin for DAPT. Patients who are treated with OAC (oral anticoagulants) should receive clopidogrel instead of ticagrelor for DAPT.
Ticagrelor is a potent platelet inhibitor with rapid onset and constant effect. Ticagrelor (loading dose of 180 mg, followed by 90 mg twice daily) has been compared to clopidogrel in patients with acute coronary syndromes with or without ST-segment elevation. Ticagrelor reduced the rate of cardiovascular death, myocardial infarction, and stroke without an increase in the risk of major bleeding but with an increase in the rate of non–procedure-related bleeding (Wallentin et al, NEJM).
Dyspnea is a common, and mostly transient, side effect of ticagrelor.
DAPT (Dual Antiplatelet Therapy)
Recommendation: DAPT is recommended during the first 12 months post-PCI. Earlier termination of DAPT is recommended if the risk of bleeding outweighs the risk of thrombosis.
Patients with chronic coronary syndromes who undergo PCI are eligible for DAPT. Aspirin is combined with one P2Y12 inhibitor up to 12 months post-PCI. The purpose of DAPT is to reduce the risk of stent thrombosis.
The risk of stent thrombosis diminishes rapidly during the first 30 days post-PCI. Yet, DAPT is recommended up to 12 months post-PCI. Premature termination of DATP (<12 months) is acceptable if the risk of serious bleeding outweighs the risk of thrombosis.
The benefits and hazards of continuing DAPT beyond 12 months remains unresolved. PEGASUS-TIMI 54 (Bonaca et al) demonstrated that ticagrelor therapy beyond 12 months, on a background of aspirin, reduced ischemic events in patients with acute MI, although at the cost of non-fatal bleeding events.
Anticoagulants
There are no data to support the use of anticoagulants in patients with chronic coronary syndromes. Studies have compared various combinations of NOAC (novel oral anticoagulants) and VKA (vitamin K antagonists), with platelet inhibitors. No combination with OAC is superior to DAPT. Rivaroxaban (LOWASA, COMPASS, GEMINI-ACS trials) on top of aspirin and clopidogrel results in fewer cardiovascular events in patients with acute coronary syndromes, but without improving overall survival.
Stopping of oral anticoagulants and platelet inhibitors before elective procedures
- NOACs should be stopped 12–48 h before elective PCI.
- Vitamin K antagonists (warfarin) may be continued during elective PCI.
- Unfractionated heparin (UFH) should be administered during PCI in patients on VKA or NOAC:
- UFH dose with continued VKA treatment: 30–50 U/kg.
- UFH dose when stopping NOAC: 70–100 U/kg.
- Aspirin should be continued during elective cardiac surgery.
- Prasugrel is stopped 7 days before elective surgery.
- Clopidogrel is stopped 5 days before elective surgery.
- Ticagrelol is stopped 3 days before elective surgery.
- NOACs (rivaroxaban, apixaban, edoxaban, dabigatran) are stopped 1-2 days before elective surgery.
Statins, ezetemibe and PCSK9 inhibitors
Recommendations:
– All patients should receive statin therapy. LDL cholesterol should drop ≥50% and to <1.4 mmol/L (<55 mg/dL). Patients who have two thrombotic events within 24 months should be treated to <1.0 mmol/L (<40 mg/dL).
– Ezetimibe is added if statins are insufficient to achieve target levels of LDL cholesterol.
– PCSK9 inhibitors are added if ezetimibe is insufficient.
Humans tolerate very low levels of cholesterol. LDL cholesterol of 0.8 mmol/L (31 mg/dL) is considered sufficient for good health. Atherosclerosis does not occur at LDL cholesterol of 0.5 mmol/L (19 mg/dL) (Libby et al, Robbinson et al).
Lowering lipid levels by means of dietary changes, exercise and weight control is recommended, although difficult to achieve. Statins, ezetemibe and PCSK9 inhibitors are potent cholesterol lowering drugs that primarily target LDL cholesterol (Ference et al). Statins lower LDL cholesterol levels through inhibition of the liver enzyme HMG-CoA reductase. Statins are potent cardioprotective drugs, with decades of data supporting their broad use (Collins et al).
Aggressive statin therapy can produce regression of atherosclerosis and, therefore, high dose statin therapy is recommended to all patients. The mainstay of statin therapy is currently atorvastatin and rosuvastatin. Simvastatin, pravastatin are less potent and cause more side effects. Lower doses are recommended to elderly patients, as well as patients with kidney or liver failure.
Follow-up of statin therapy is suitable 2 months after initiation of therapy. LDL cholesterol should drop at least 50% and to <1.4 mmol/L (<55 mg/dL). Patients who have two thrombotic events within 24 months should be treated to <1.0 mmol/L (<40 mg/dL).
If statins are insufficient to reach the target level for LDL cholesterol, then ezetimibe may be added. Ezetimibe reduces the risk of cardiovascular events. Ezetimibe may also be given to patients who do not tolerate statins. Ezetimibe is considerably more expensive than statins.
PCSK9 inhibitors (evolocumab and alirocumab) provide very effective LDL reduction, and also additional reduction in the risk of cardiovascular events, on top of statin therapy. However, PCSK9 inhibitors do not affect survival and are considerably more expensive than statins and ezetimibe.
The JUPITER trial reported that statins can induce diabetes. Subsequent sub-analyses demonstrated that statins accelerate the onset of diabetes (on average by 18 months) in individuals who would likely develop diabetes regardless of statin therapy (Ridker et al).
Dietary effects on lipid levels
A strict low-fat diet provides a modest reduction in blood fats and is insufficient to manage cholesterol levels.
Exercise
All patients are recommended 30-60 minutes of daily exercise. Exercise improves cardiovascular outcomes. Collateral arteries, endothelial function and the atherosclerotic process are all affected favorably by exercise.
Revascularization in stable angina pectoris
Revascularization by PCI or CABG (coronary artery bypass grafting) may improve survival, alleviate symptoms, reduce ischemia, increase functional capacity and quality of life in individuals with coronary artery disease (Windecker et al, Knuuti et al). Revascularization is considered if optimal medical therapy is insufficient to achieve the treatment goals, or if prognosis can be improved.
Decision on revascularization require functional and anatomical evaluation of the coronary arteries, the purpose of which is to determine the extent and hemodynamic significance of stenoses. Figure 5 shows the decision tree recommended by the European Society for Cardiology.

The choice between PCI and CABG remains debatable, although it is consensus that the following patients benefit more from CABG:
- Individuals with diabetes.
- Individuals older than 65 years.
- Individuals with multivessel disease, or left main disease, particularly high-risk individuals.
With the exception of these three groups, PCI and CABG appears to be equal. Adding elective PCI to OMT in remaining patients does not confer a survival benefit (The COURAGE Trial).
References
Knuuti et al: 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal (2019). KNUUTI ET AL IS MAIN SOURCE OF THIS CHAPTER.
Williams RP, Manou-Stathopoulou V, Redwood SR, Marber MS. ‘Warm-up Angina’: harnessing the benefits of exercise and myocardial ischaemia. Heart 2014;100:106 114.
Fisher et al: Rapid regression of atherosclerosis: insights from the clinical and experimental literature. Nature Clinical Practice Cardiovascular Medicine volume 5, pages91–102(2008)Cite this article
Peter Libby et al. Atherosclerosis. Nature Reviews Disease Primers volume 5, Article number: 56 (2019).
Juarez-Orozco et al. Impact of a decreasing pre-test probability on the performance of diagnostic tests for coronary artery disease. Eur Heart J Cardiovasc Imaging 2019.
Ference et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017.
Arbab-Zadeh et al. Acute coronary events. Circulation (2012).
Collet et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal (2020).
Ibanez et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal (2018).
Collins et al. Interpretation of the evidence for the efficacy and safety of statin therapy. The Lancet 2016.
Aradi D et al. Working Group on Thrombosis of the European Society of Cardiology. Expert position paper on the role of platelet function testing in patients undergoing percutaneous coronary intervention. Eur Heart J 2014;35:209-215.
Robinson J al. Safety of very low low-density lipoprotein cholesterol levels with alirocumab: pooled data from randomized trials. J Am Coll Cardiol. 2017.
Windecker et al. Revascularisation versus medical treatment in patients with stable coronary artery disease: network meta-analysis. BMJ 2014.
Gavazzi et al: Significance of the walk-through angina phenomenon during exercise testing. Cardiology. 1986;73(1):47-53.
Mills EJ, Thorlund K, Eapen S, Wu P, Prochaska JJ. Cardiovascular events associated with smoking cessation pharmacotherapies: a network meta-analysis. Circulation 2014;129:28-41.
Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross L, Goniewicz M, Wu Q, McRobbie HJ. A randomized trial of E-cigarettes versus nicotine-replacement therapy. N Engl J Med 2019;380:629-637.
Shai et al. Weight Loss with a Low-Carbohydrate, Mediterranean, or Low-Fat Diet List of authors. NEJM 2008.
Dehghan et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. The Lancet 2017.
Mente et al. Association of dietary nutrients with blood lipids and blood pressure in 18 countries: a cross-sectional analysis from the PURE study. The Lancet 2017.
Fox K et al. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet 2008.
Fox K et al: Ivabradine in stable coronary artery disease without clinical heart failure. N Engl J Med 2014;371:1091-1099.