Regional Myocardial Contractile Function: Wall Motion Abnormalities
Echocardiographic assessment of regional contractile function
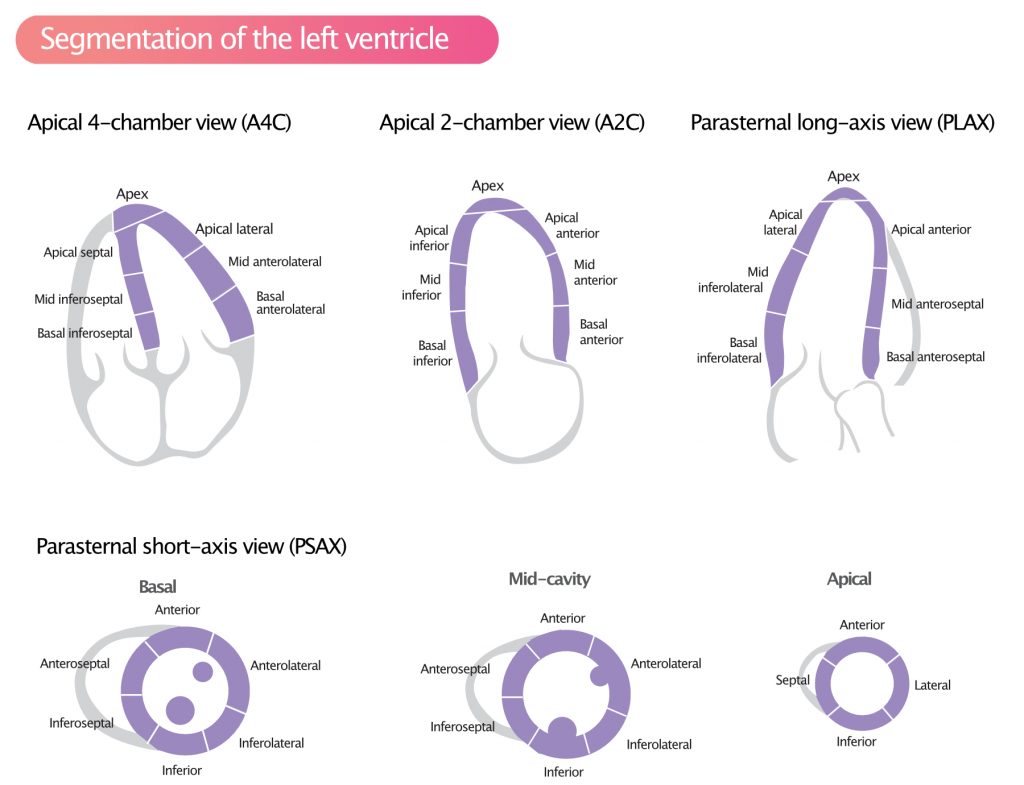
Systolic ventricular function is one of the strongest predictors of total and cardiovascular mortality. Previous chapters have discussed several methods for assessment of global and regional ventricular function. Assessment of regional wall motion is an integral aspect of virtually every echocardiographic examination. Wall motion is assessed in each segment of the left ventricle (Figure 1; refer to Segments of the Left Ventricle). Regional wall motion abnormalities are defined as regional abnormalities in contractile function. Ischemic heart disease is the most common cause of wall motion abnormalities. Assessment of wall motion abnormalities is particularly important in the setting of chronic or acute coronary artery disease.
All types of ischemia–chronic, acute, or subacute–lead to regional abnormalities in contractile function. The abnormalities affect the myocardial area supplied by the arteries distal to the occlusion or stenosis. If the ischemia persists for 20 minutes, myocardial infarction ensues, resulting in permanent wall motion abnormalities.
Note that the terms ischemic heart disease (IHD), coronary heart disease (CHD), and coronary artery disease (CAD) are used interchangeably throughout this text.
Wall motion abnormalities in ischemic heart disease
In the setting of stable ischemic heart disease, an atherosclerotic plaque causes ischemia when myocardial oxygen demand exceeds the oxygen supply. The most characteristic manifestation of ischemic heart disease is angina pectoris developing during physical activity; myocardial oxygen demand increases during physical activity, but an atherosclerotic plaque may prevent oxygen supply from increasing in parallel with oxygen demands. Depending on several factors–including the severity of the stenosis/occlusion, microvascular function, myocardial oxygen extraction, presence of collateral circulation, etc–ischemia may also develop during resting conditions. Indeed, in patients with ischemic heart disease, the majority of all ischemic episodes are asymptomatic (refer to The Ischemic Cascade). Acute coronary syndromes occur when atherosclerotic plaques rupture or erode, leading to atherothrombosis and occlusion. This causes severe ischemia and the vast majority of patients experience angina pectoris.
Myocardial ischemia: Supply-demand imbalance vs. lack of supply
In clinical practice, ischemia is often described as a consequence of an imbalance between oxygen demand and supply. According to this theory, ischemia occurs when the oxygen demand exceeds the oxygen supply. However, experimental and clinical studies have shown that myocardial metabolism, and thus contractility, is tightly coupled to oxygen supply. The myocardium is capable of upregulating or downregulating metabolism (i.e contractility) according to oxygen supplies. Consequently, reduced oxygen supply would not result in ischemia, since the myocardium adapts and downregulates metabolism to avoid developing ischemia. According to this theory, ischemia occurs only if there is an absolute lack of oxygen (Heusch et al).
Ischemic myocardium exhibits wall motion abnormalities
In the setting of ischemia, myocardial contractility is downregulated or completely ceased. The ischemic area will immediately display wall motion abnormalities. This is useful in emergency medicine since the presence of wall motion abnormalities in a patient with chest pain strongly suggests myocardial ischemia as the underlying cause of the symptoms.
The degree and extent of wall motion abnormalities correlate well with the severity and extent of ischemia. In the setting of moderate ischemia, the myocardium becomes hypokinetic, meaning that the ischemic segments contract less than the surrounding segments. During pronounced ischemia, the myocardium becomes akinetic (contractions have ceased). Akinetic myocardium is also called stunned myocardium. Myocardial stunning may normalize completely if the ischemia is alleviated before infarction ensues.
Echocardiography for assessment of wall mobility
Regional wall motion can be assessed with a scoring system developed by the American Society for Echocardiography (ASE). The left ventricle is divided into 17 segments (Figure 1) and each segment should be assessed for contractility (motion) using the following scoring system:
| Points | Abnormality |
| 1 | Normal motion |
| 2 | Hypokinesia |
| 3 | Akinesia |
| 4 | Dyskinesia |
Wall Motion Score Index (WMSI)
The Wall Motion Score Index (WMSI) is calculated by dividing the number of points by 17. If all segments move normally, the ratio is 1 (17 divided by 17). WMSI >1.7 is typically associated with heart failure.
The most frequent cause of regional wall motion abnormality is ischemic heart disease. Myocardial infarction may cause regional hypokinesia, akinesia or dyskinesia. The distribution of wall motion abnormalities should match the territory of a coronary artery.
Unfortunately, echocardiography can not determine whether wall motion abnormalities are new or old. This implies that echocardiography can not differentiate acute ischemia and old infarctions. However, the morphology of the myocardium may provide guidance. Scar tissue (i.e myocardial infarction) becomes thinner and appears brighter (echogenicity is higher) in the ultrasound image. Thus, wall motion abnormalities affecting thinner and brighter myocardium suggests infarction as the underlying cause.
Other causes of regional wall motion abnormalities
Although myocardial ischemia is the most common cause of wall motion abnormalities, there are numerous other causes, listed in Table 1. The most common among these is left bundle branch block (LBBB).
| Table 1. Differential diagnoses for regional wall motion abnormalities |
| Left bundle branch block (LBBB) |
| Pacemaker |
| Pre-excitation |
| Premature ventricular beats |
| Constrictive pericarditis |
| Right ventricular strain |
| Non-ischemic dilated cardiomyopathy (DCM) |
| Takotsubo syndrome |
| Sarcoidosis |
| Hemochromatosis |
If wall motion abnormalities involve more than one arterial territory, non-ischemic causes should be suspected (Table 1). Furthermore, normal thickening of the myocardium also suggests non-ischemic causes.
