Methods for assessing systolic function (contractile function)
Several echocardiographic measurements are available to assess left ventricular systolic function. These methods elucidate slightly different aspects of systolic function and their combined use allows for careful mapping of systolic function. It is important to be familiar with the advantages and disadvantages of each method. An overview of available methods follows. Each method is discussed in detail in subsequent chapters.
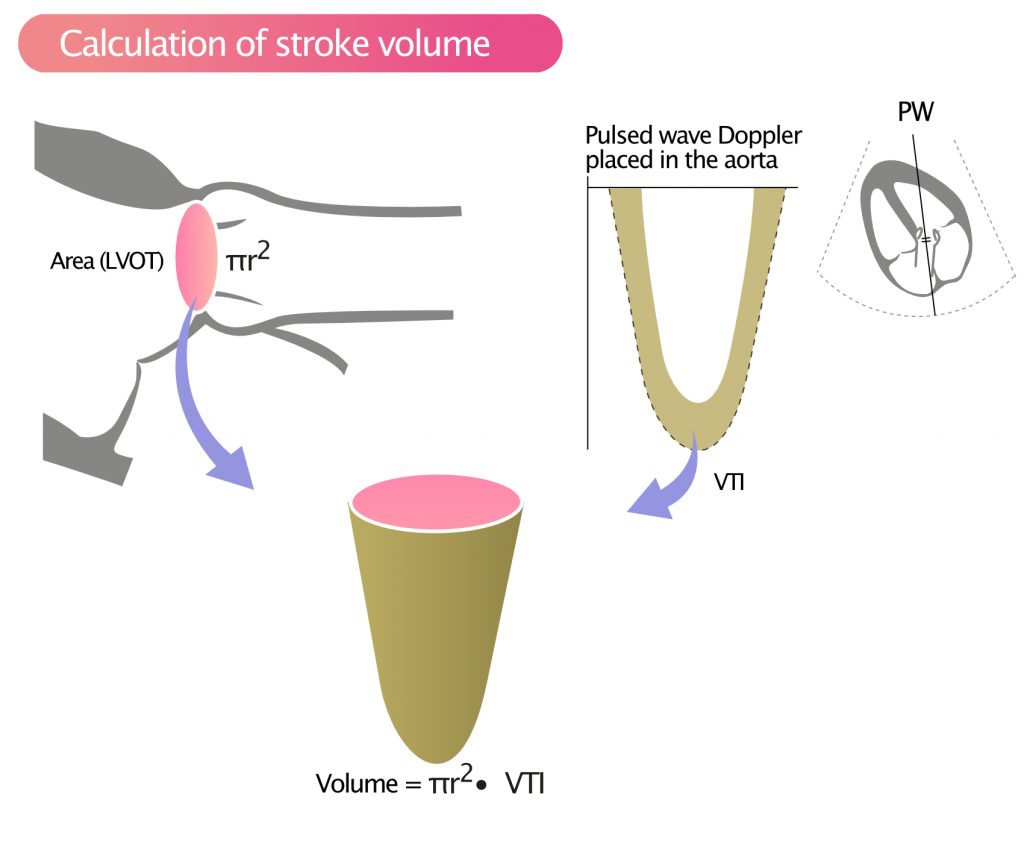
Stroke volume (SV)
Stroke volume is the volume of blood pumped from the left ventricle into the aorta during systole. It is easily calculated by measuring VTI (Velocity Time Integral), using pulsed wave Doppler, in the aortic valve. The stroke volume is the product of VTI and area of the LVOT, as illustrated in Figure 1.
Cardiac output (CO)
Cardiac output is the product of stroke volume (SV) and heart rate (HR).
CO = HR · SV
Cardiac Index (CI)
Cardiac Index (CI) is the ratio between cardiac output (CO) and body surface area (estimated by weight and height). Thus, cardiac index is cardiac output normalized to body surface area. The ultrasound system calculates body surface area using the patient’s sex, weight and height.
CI = CO / BSA
BSA = Body Surface Area (m2)
Ejection fraction (EF)
Ejection fraction is the fraction of the end-diastolic volume (EDV, i.e blood volume in the ventricle at the end of diastole) that is pumped out during systole. Currently, two-dimensional (2D) echocardiography for calculation of ejection fraction is the dominant method for assessing left ventricular function (systolic function). It should be noted, however, that three-dimensional (3D) echocardiography offers greater precision in the calculation of ejection fraction, and 3D measurements will presumably replace 2D measurements in the future. Cardiac MRI (magnetic resonance imaging) is considered the gold standard for the calculation of ejection fraction.
Recommended chapter: Ejection fraction
Ejection acceleration time (EAT)
Ejection acceleration time measures the maximum systolic velocity (m/sec) in the LVOT. This parameter correlates well with left ventricular systolic function.
EAT = vmax/time
Fractional shortening (FS)
Fractional shortening (FS) is calculated by measuring the change (% reduction) in left ventricular diameter during systole. It is considered a poor measure of systolic function; it is only reliable if the left ventricle has normal geometry and no significant wall motion abnormalities. Fractional shortening can be measured in M-mode and 2D.
FS = (LVEDD – LVESD)/LVEDD
LVEDD = left ventricular end-diastolic diameter; LVESD = left ventricular end-systolic diameter;
The fraction is multiplied by 100 to obtain percentage (%).
| Normal FS | >25% (M-Mode) |
| >18% (Direct 2-D measurement) |
Tissue Doppler
Tissue Doppler records the speed and direction of myocardial motion. This is possible because myocardium also reflects ultrasound waves. In order to analyze myocardial motion, the ultrasound system must filter out all sound waves reflected by other structures, notably sound waves reflected by blood. This is achieved by filtering out signals with low amplitude and high velocity; such signals represent reflections from blood flow. Instead, the ultrasound system focuses on sound waves with high amplitude and low velocity; these waves are reflected from myocardium.
Tissue Doppler can also be used to measure the velocity of the mitral annulus, as it travels from the base to the apex during systole. Mitral annulus velocity correlates well with ejection fraction, stroke volume and is thus a measure of systolic function.
Strain and strain rate
Myocardium deforms during systole and diastole. The deformation is due to contraction and relaxation, which results in myocardium moving and deforming. Strain is the echocardiographic term for deformation. Strain and strain rate measure the extent and velocity of myocardial deformation. These parameters can be assessed using tissue Doppler or speckle tracking. The latter method is the dominating for assessing deformation.
dP/dt
In the setting of mitral regurgitation, left ventricular systolic function can be estimated by studying the acceleration of the regurgitant jet (Figure 2). The better the systolic function, the greater the increase in left ventricular systolic pressure, and, thus, the greater the acceleration in the regurgitant jet. Hence, dP/dT is a proxy for the capacity of the left ventricle to generate pressure during systole. It represents a marker of global contractile function.
dP/dT is measured by placing continuous wave Doppler in the MR jet (mitral regurgitation jet) during the isovolumetric contraction (i.e. the contraction occurring between mitral valve closure and aortic valve opening), as seen in Figure 2. Left atrial pressure is constant during this phase, which implies that the acceleration in MR jet speed is due to increase in left ventricular pressure.
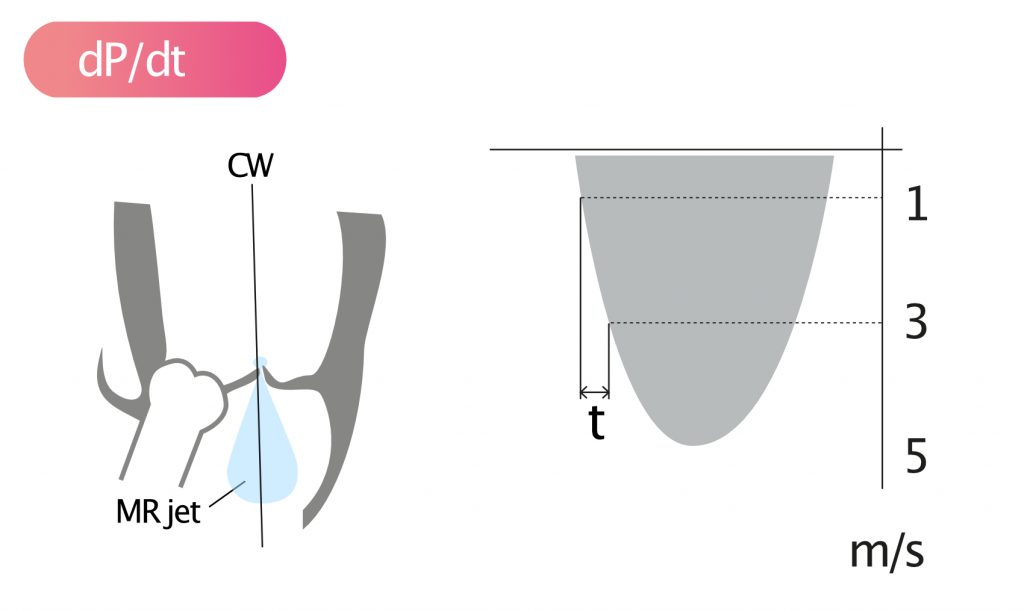
More specifically, dP/dt is derived by measuring the time interval (s) elapsing for the MR jet to accelerate from 1 m/s to 3 m/s. Then, the constant 32 is divided by the time interval in order to approximate left ventricular pressure :
dP/dt = 32/t
t=time interval (s)
dP/dt has the unit mmHg/s.
| Variable | Definition |
| T | Time (1 to 3 m/sec MR) (seconds, s) |
| dP/dt | dP/dt (mmHg/s) |
| Normal | ≥1200 mmHg/s |


