The mitral valve
The mitral valve separates the left atrium and the left ventricle. The valve is attached to the mitral annulus, which is continuous with annulus fibrosus (the fibrous ring). The mitral valve has an anterior leaflet and a posterior leaflet. The anterior leaflet has a semi-circular shape and is firmly attached to two fifths of the circumference of the mitral annulus. The aorto-mitral curtain separates the aortic valve and the anterior leaflet of the mitral valve. The anterior leaflet is anatomically divided into three segments referred to as A1 (anterior segment), A2 (middle segment), and A3 (posterior segment) (Figure 1). The posterior leaflet of the mitral valve has a semilunar shape and is attached to three fifths of the annular circumference. The posterior leaflet generally has two distinct indentations which divide it into three scallops, P1 (anterior or medial scallop), P2 (middle scallop), and P3 (posterior or lateral scallop).
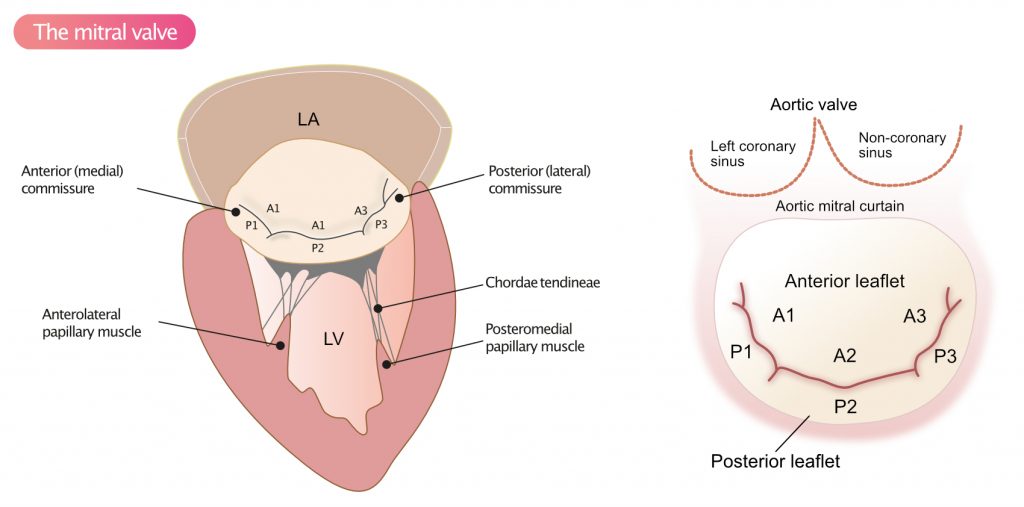
The leaflets are connected to the papillary muscles via chordae tendineae (Figure 1). The anterolateral papillary muscle receives blood supply from the left anterior descending artery (LAD) and the left circumflex artery (LCX), whereas the posteromedial papillary muscle receives blood supply from either LCX or the right coronary artery (RCA). For details, refer to chapter The Coronary Arteries.
Mitral valve disease
A wide range of conditions may cause mitral valve disease, which results in changes in the pressure-volume relationships in the ventricle and the atrium. Pressure and/or volume overload causes dilation of the ventricle and/or atrium, which compensates by dilating. The dilation may also lead to dilatation of the mitral annulus, which further impairs coaptation of the leaflets and thus causes mitral regurgitation. The term coaptation is used to describe how well the leaflets meet and close the valve during systole. Poor coaptation leads to regurgitation.
Mitral stenosis
Mitral stenosis is defined as a narrowing of the mitral valve orifice. There are many causes of mitral stenosis, the most common of which are rheumatic heart disease, congenital malformations, radiation complications, metastases, myxoma, cardiac thrombi, etc (Table 1).
Most causes of mitral stenosis yield a progressive narrowing of the mitral valve. Mitral stenosis is a slowly progressing disease that eventually causes heart failure. Mitral stenosis typically becomes symptomatic at rest when the valve area is reduced to 1.5 cm2. During physical activity, mitral stenosis may become symptomatic already at 2.5 cm2. A normal mitral valve has an area of 4 to 6 cm2. A valve area <1 cm2 indicates severe mitral stenosis.
| Table 1. Causes of mitral stenosis |
| Rheumatic heart disease |
| Congenital mitral stenosis |
| Calcification of the mitral valve |
| Complications to radiation therapy |
| Mucopolysaccharidosis |
| Carcinoid tumor |
| Systemic lupus erythematosus (SLE) |
| Rheumatoid arthritis (RA) |
| Iatrogenic stenosis after mitral valve surgery |
| Myxoma obstructing outflow from the left atrium |
| Atrial thrombus obstructing atrial outflow |
| Endocarditis |
Hemodynamic consequences of mitral stenosis
Mitral stenosis hinders atrial emptying. This results in an increase in left atrial pressure (LAP), which gradually leads to atrial hypertrophy and dilation. Atrial dilation causes a significantly increased risk of atrial fibrillation. The increase in left atrial pressure may also propagate backward to the pulmonary circulation, causing pulmonary hypertension (PH). Additionally, pulmonary hypertension can propagate further backward to the right ventricle and right atrium, leading to right heart hypertrophy, dilation and ultimately right heart failure.
Echocardiography in mitral stenosis
Echocardiographic assessment of mitral stenosis includes visual and 2D imaging, as well as Doppler measurements to assess the degree of stenosis and evaluation of complications.
Visual assessment in 2D
- Is the mitral valve normal, thickened, calcified or are there vegetations?
- Are both leaflets moving normally?
- Does leaflet doming occur during diastole?
- Can the chordae tendineae be discerned? Are the strands calcified or fused?
Classification of mitral stenosis severity
The severity of mitral stenosis is classified on the basis of valve area and pressure gradients across the valve. Table 2 presents criteria for classification of disease severity. The required measurements and techniques are discussed below.
Table 2. Criteria for echocardiographic diagnosis of MS severity
| Mild | Moderate | Severe | |
|---|---|---|---|
| Mean pressure decrease | <5 mm Hg | 6–10 mm Hg | >10 mm Hg |
| Pressure half-time | <139 ms | 140–219 ms | ≥220 ms |
| Valve area | 1.6–2.0 cm2 | 1.5–1.0 cm2 | <1.0 cm2 |
Calculation of valve area
Valve area is a key parameter in the assessment of disease severity. The smaller the valve orifice, the more pronounced the stenosis. There are three methods to calculate valve area.
Method 1: Direct measurement of valve area in PSAX
The valve area can be measured directly in the parasternal short-axis view (PSAX) during diastole. The ultrasound beam should be positioned so as to intersect the leaflet tips, otherwise, the valve area may be overestimated (Figure 2).

Method 2: Pressure Half Time (PHT)
Using continuous wave Doppler, placed in the mitral valve, the PHT of the E wave is measured. PHT is the time it takes for the pressure difference between the atria and ventricles to halve. Table 2 presents grading criteria for PHT. The valve area (MVA, Mitral Valve Area) can then be estimated by the formula:
MVA = 220/PHT
The same Doppler measurement is used to calculate the mean pressure gradient across the mitral valve (ΔP, mmHg). Note that the formula cannot be used in the setting of prosthetic valves, atrial septal defect, severe aortic regurgitation or very high left ventricular filling pressures.
Method 3: The continuity equation
According to the continuity equation, the amount of blood flowing through the mitral valve during diastole must be equal to the volume flowing through LVOT during systole. Hence, MVA (mitral valve area) can be calculated as follows:
MVA = 𝛑 × (DLVOT/2)2 × (VTILVOT/VTImitral)
D = diameter in cm.
VTILVOT measured with pulsed Doppler i LVOT.
VTImitral measured with continuous Doppler in the mitral valve.
The above formula should not be used in the setting of atrial fibrillation, significant mitral regurgitation or aortic regurgitation.
Mean and maximum pressure gradient across the mitral valve
The mean pressure gradient (difference) and maximum pressure gradient are calculated using continuous wave Doppler through the mitral valve (apical view). The maximum pressure gradient is calculated using the maximum velocity and Bernoulli’s simplified formula, as follows:
ΔPmax = 4vmax2
Mean pressure gradient (ΔPmean) reflects the mean pressure difference between the left atrium and ventricle during diastole and it is calculated using the obtained VTI. Note that the mean pressure gradient is affected by heart rate, filling time, cardiac output and mitral regurgitation, if present. The heart rate should always be noted.
Pulmonary arterial pressure (PASP, pulmonary artery systolic pressure)
PASP and Mean Pulmonary Arterial Pressure (MPA) should be measured.
If the patient has atrial fibrillation, measurements should be made on 5 consecutive cardiac cycles and the mean values of each parameter used to make the calculations.
In addition to the above parameters, the size of the left atrium should also be measured to clarify whether the atrium is dilated.
