Predicting sudden cardiac arrest
The purpose of discovering and measuring risk factors is to obtain estimates of risk, tailor management according to the risk and monitor risk prospectively. Strong risk factors serve as useful predictors in prediction models. Targeting risk factors has been very successful in the primary and secondary prevention of atherosclerotic cardiovascular disease, both at the population and individual levels. Several prediction models have been developed and validated for the prediction of heart failure, coronary artery disease, acute coronary syndromes and stroke (Steyerberg et al). Achieving this has been significantly more difficult for the prediction of cardiac arrest.
Sudden cardiac arrest is the most lethal manifestation of cardiovascular disease, accounting for 50% of all cardiovascular deaths (Tsao et al). A recent meta-analysis showed that survival to hospital discharge is 8.8% and survival to 30 days is 10.7% in out-of-hospital cardiac arrest (Yan et al). The low survival reflects the sudden and hyperacute nature of the condition. This has prompted researchers to develop strategies and tools for long-term prevention of cardiac arrest. Unfortunately, these efforts have not borne fruit. Our current ability to predict cardiac arrest remains poor at best.
A key explanation for this is the stochastic nature of sudden cardiac arrest and death. The randomness of the event has puzzled researchers for over 80 years. This was expressed in 1961 by Beck et al in the Journal of American Medical Association (JAMA):
[…] Of every 10 such victims, the heart in 6 or 7 showed no recent disease in coronary arteries or in heart muscle. In other words, the heart today is anatomically the same as it was yesterday except that an electrical charge developed which fibrillated the heart. This electrical factor came and killed and disappeared and was not found in the dead heart. The cause of death in these victims is not explained on the basis of morbid anatomy. This is not a new experience for either the pathologist or the internist. That there is something lacking in our understanding of this problem is indicated when death occurs after the victim was given “a clean bill of health” and no explanation of death […]
Only in a small and highly selected sub-group of patients can reasonable predictions be made (which guides decisions regarding the implantation of ICDs [implantable cardioverter defibrillator]). Our inability to predict cardiac arrest is evident in many ways. Some examples follow:
- Modern ICDs are capable of successfully defibrillating 99% of ventricular tachyarrhythmias. Theoretically, ICDs could treat 99% of all cardiac arrests caused by ventricular tachyarrhythmias (which are the majority of cases). Yet, only a negligible fraction of all victims of cardiac arrest have an ICD.
- Half of all victims of cardiac arrest have no previous history of cardiovascular disease. Sudden cardiac death accounts for 40–70% of all deaths from coronary artery disease (Kannel et al, Demirovic et al).
As described by Myerburg et al and Marijon et al, long-term prevention of cardiac arrest at the population level is very difficult. Future efforts may be more successful by focusing on near-term prediction using smart devices and emerging technologies (Marijon et al).
The stochastic nature (randomness) of sudden cardiac arrest is in some aspects similar to acute coronary syndromes. An acute coronary syndrome is the result of a perfect storm scenario, where disruption of an atherosclerotic plaque coincides with a pro-thrombogenic moment in thrombocytes, coagulation factors, endothelial function, etc. The perfect storm implies that plaque disruption occurs when pro-thrombogenic factors outweigh pro-thrombolytic factors. The balance between pro-thrombogenic and pro-thrombolytic factors determines whether atherothrombosis occurs, and these factors vary from minute to minute. Only a minority of all plaque disruptions result in acute coronary syndromes; the majority of plaque disruptions are asymptomatic (Arbab-Zadeh et al). The emergence of ventricular tachyarrhythmias follows the same principles, where pro-arrhythmogenic factors are counteracted by anti-arrhythmogenic factors. Examples of such factors include electrolyte concentrations, sympathetic tone, degree of myocardial ischemia, QT time, etc., (Myerburg et al).
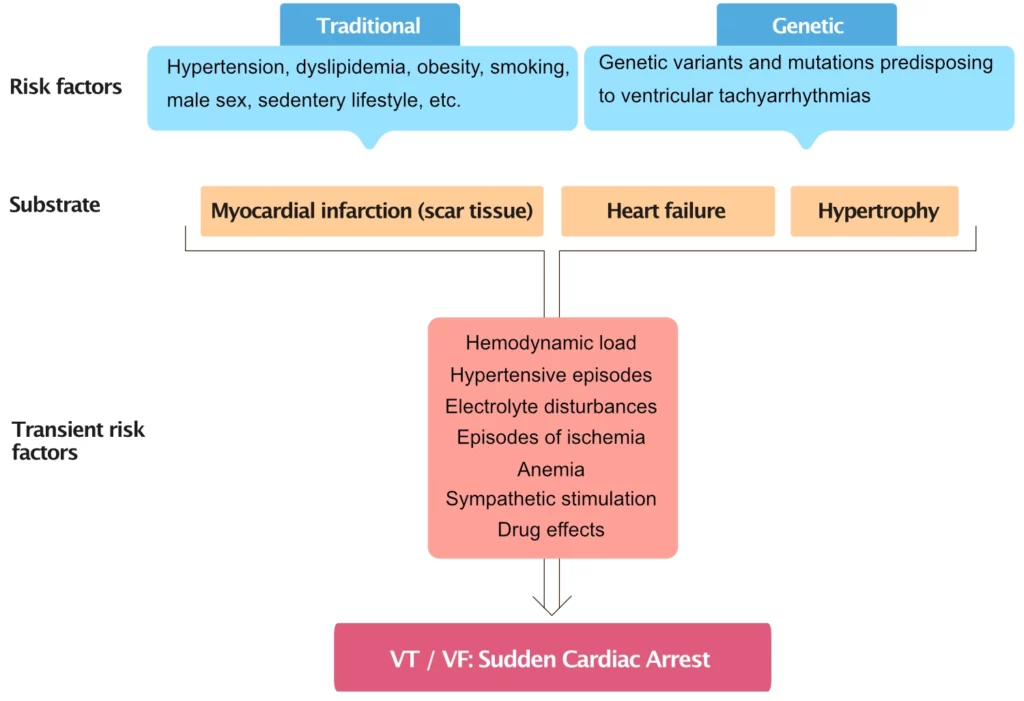
The multifactorial processes culminating in sudden cardiac arrest or death typically require acquiring an arrhythmogenic substrate, capable of generating tachyarrhythmias during specific (often transient) conditions and states, as depicted in Figure 1.
Traditional cardiovascular risk factors
Traditional cardiovascular risk factors (diabetes, hypertension, dyslipidemia, sedentary lifestyle, abdominal obesity, etc.) are also risk factors for sudden cardiac arrest. The risk of sudden cardiac arrest is clearly associated with the number of risk factors. Participants in the highest-risk decile in the Framingham study had a 14-fold increased risk of sudden cardiac death (compared with the lowest-risk decile). These risk factors cause the underlying conditions (substrates) for cardiac arrests, such as myocardial infarction, heart failure, or other forms of ventricular dysfunction.
These risk factors have been successfully targeted through primary prevention, which is likely to have reduced the incidence of cardiac arrests by reducing the incidence of acute myocardial infarction (Nabel et al).
Discordance between relative and absolute risk
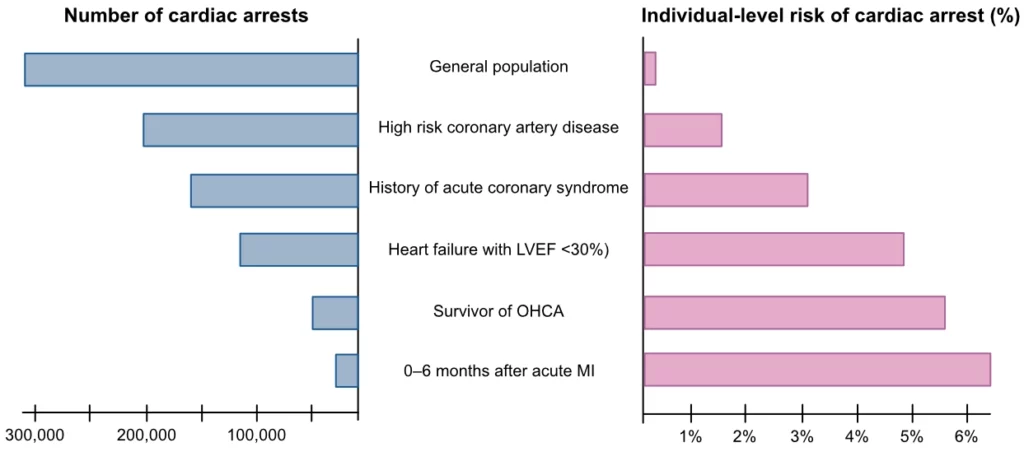
One of the challenges in identifying individuals with high risk is the marked discordance between the relative risk and population attributable fraction (PAF). This is depicted in Figure 2 (adapted from Myerburg et al), which demonstrates that the vast majority of all cardiac arrests occur in the general population, among individuals with low relative risk of cardiac arrest. The relative risk of cardiac arrest is very low in the general population (0,1% per year), the total number of cardiac arrests in the general population far exceeds the number of arrests in high-risk groups. The latter, represented primarily by individuals with coronary artery disease and heart failure are at high relative risk of cardiac arrest but amount to few cases (due to the small size of these sub-populations).
Overview of risk factors for cardiac arrest
- Age — The risk of cardiac arrest is high in the first year of life and after 45 years of age. Starting at the age of 35 years, coronary artery disease is the leading cause of cardiac arrest.
- Male sex — Men are at higher risk of cardiac arrest than women across the lifespan. Approximately 65% of all cardiac arrests occur among men.
- Circadian variation — The risk of cardiac arrest is higher in the morning, on Mondays, and during the winter months. Cold weather is also a risk factor, as is heatstroke.
- Environment — Air pollution increases the risk of acute myocardial infarction and thus cardiac arrest.
- Cardiovascular Disease — Individuals with coronary heart disease (stable angina or manifest myocardial infarction), heart failure, cardiomyopathy, or valvular heart disease are at increased risk of ventricular arrhythmias. In the case of acute myocardial infarction, the risk of ventricular arrhythmias is highest during the first hour, whereafter the risk subsides rapidly.
- Cardiovascular Risk Factors — Hypertension, diabetes, smoking, sleep apnea, obesity, and dyslipidemia, etc., are also risk factors for cardiac arrest.
- Moderate alcohol consumption likely reduces the risk of cardiac arrest, which can be explained by the association between moderate alcohol consumption and acute myocardial infarction (The GBD Study).
- Genetics and syndromes — Brugada syndrome, congenital or acquired long QT syndrome, early repolarization syndrome, catecholaminerg polymorphic ventricular tachycardia (CPVT) and catecholaminerg polymorphic ventricular fibrillation (CPVF) are hereditary conditions that increase the risk of sudden cardiac arrest.
Left ventricular ejection fraction
The strong association between left ventricular ejection fraction (LVEF) and the risk of sudden cardiac arrest has been recognized for decades (Bigger et al). LVEF is arguably one of the strongest predictors of sudden death. The MADIT II trial demonstrated that implantation of an ICD in individuals with LVEF <30% and a history of acute myocardial infarction reduced mortality by 31%. Subsequent randomized trials demonstrated similar results, leading to broad recommendations for ICD implantation in patients with LVEF <30%. Such broad recommendations inevitably increase the number needed to treat (NNT). Indeed, LVEF is an imperfect predictor of cardiac arrest. For example, among individuals with heart failure, the mortality rate is lower among those in NYHA class I-II (better ventricular function) as compared with NYHA class III-IV (worse ventricular function), but the proportion of deaths that are sudden is higher in NYHA class I-II (Moss et al, Packer et al). Moreover, the predominating method for measuring LVEF – i.e. echocardiography – is less reproducible than cardiac MRI or cardiac CT.
Other risk factors for cardiac arrest
- Exercise capacity (measured as VO2 max) is considered a strong predictor of cardiovascular death.
- Physical activity should not be considered a risk factor for cardiac arrest. The risk of suffering a cardiac arrest during physical activity is extremely small (<1/1000000). However, untrained individuals who make sudden vigorous physical exertions are at a slightly increased risk of cardiac arrest (Albert et al). Untrained individuals should increase their exercise load gradually over several months.
- Intraventricular conduction defects (left bundle branch block, nonspecific conduction defects) constitute risk factors for cardiac arrest.
- Myocardial infarction size affects the risk of cardiac arrest during the acute, subacute, and chronic phase (Goldberger et al). Infarctions resulting in heart failure are particularly prone to developing cardiac arrest.
- Monomorphic non-sustained ventricular tachycardia (VT) and ventricular extrasystoles are considered benign arrhythmias if the patient does not have structural heart disease.
- Polymorphic VT is a strong risk factor for cardiac arrest.
- Occassionally frequent ventricular extrasystoles are a manifestation of coronary heart disease.
- Ventricular extrasystoles and non-sustained VT induced by physical exertion indicate an increased risk of cardiac arrest.
- Frequent ventricular extrasystoles (>10/h) after myocardial infarction also indicates a risk of cardiac arrest.
References
Myerburg RJ, Junttila MJ. Sudden cardiac death caused by coronary heart disease. Circulation. 2012.
Myerburg RJ, Castellanos A. Cardiac arrest and sudden cardiac death. Man DL, Zipes DP, Libby P, Bonow RO. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 10th ed. Elsevier.
Myerburg RJ, Kessler KM, Castellanos A. Sudden cardiac death: structure, function, and time-dependence of risk. Circulation 1992;85(suppl I):1–2,1–10.
Yoshinaga M, Kucho Y, Nishibatake M, et al. Probability of diagnosing long QT syndrome in children and adolescents according to the criteria of the HRS/EHRA/APHRS expert consensus statement. Eur Heart J. 2016.
A Tale of Coronary Artery Disease and Myocardial Infarction List of authors. Elizabeth G. Nabel, M.D., and Eugene Braunwald, M.D. A Tale of Coronary Artery Disease and Myocardial Infarction List of authors. Elizabeth G. Nabel, M.D., and Eugene Braunwald, M.D.
Albert CM, Mittleman MA, Chae CU, et al. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000.
Chugh SS, Reinier K, Singh T, et al. Determinants of prolonged QT interval and their contribution to sudden death risk in coronary artery disease: The Oregon Sudden Unexpected Death Study. Circulation. 2009.
Towards better clinical prediction models: seven steps for development and an ABCD for validation Ewout W. Steyerberg, Yvonne Vergouwe European Heart Journal, Volume 35, Issue 29, 1 August 2014, Pages 1925–1931, https://doi.org/10.1093/eurheartj/ehu207
Demirovic J. Risk factors in the incidence of sudden cardiac death and possibilities for its prevention. Doctoral Thesis, University of Belgrade Press, Belgrade, YU. 1985.
Myerburg RJ. Implantable cardioverter-defibrillators after myocardial infarction. N Engl J Med. 2008.
Goldberger JJ, Buxton AE, Cain M, et al. Risk stratification for arrhythmic sudden cardiac death: identifying the roadblocks. Circulation. 2011.
Bigger JT, Fleiss JL, Kleiger R, Miller JP, Rolnitzky LM. The relationships among ventricular arrhythmias, left ventricular dysfunction, and mortality in the 2 years after myocardial infarction. Circulation 1984;69:250–258. 46. Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346:877–883.
