Cardiac arrest during pregnancy and childbirth
All healthcare units capable of managing pregnant women in cardiac arrest should engage in specialized clinical training to manage cardiac arrest during pregnancy. Upon recognition of a cardiac arrest in a pregnant individual, either within or outside the hospital, prompt communication with an obstetrician and neonatologist is critical. Cardiopulmonary resuscitation (CPR) should generally adhere to the standard adult guidelines, encompassing chest compressions, ventilation, pharmacological interventions, and defibrillation according to adult recommendations. Electrode pads should be positioned as standard, and defibrillation energy levels should remain consistent with those used for non-pregnant adults. The fetus is not harmed by defibrillation, amiodarone, or adrenaline (epinephrine).
In the event of a cardiac arrest in a pregnant patient, immediate consultation with an obstetrician, neonatologist, and anesthesiologist is essential.
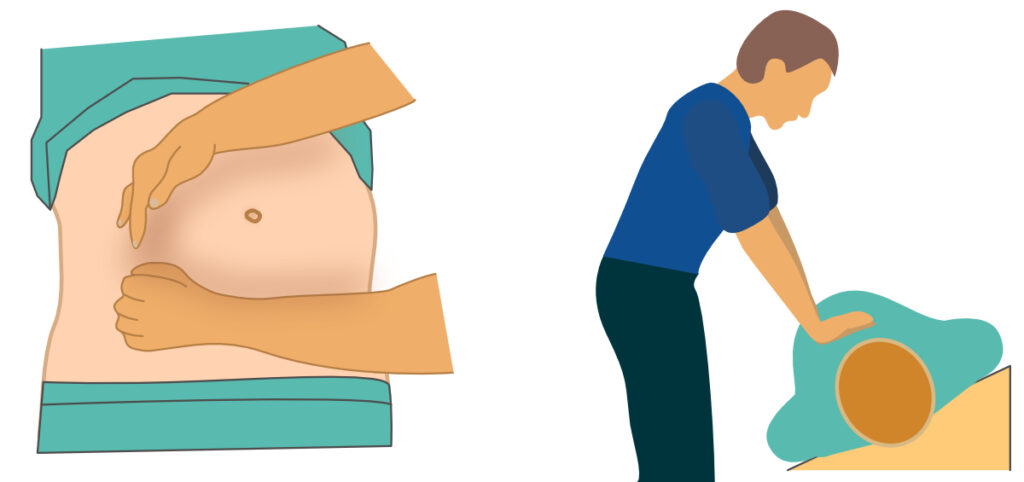
A large uterus exerts pressure on the descending aorta and vena cava inferior. The pressure in the vena cava inferior is very low, such that the vein can be fully compressed in the supine position in a cardiac arrest. For women beyond the 20th week of pregnancy, or when the fundal height surpasses the umbilicus, the uterus should be manually displaced to the woman’s left side (Figure 1). Additional offloading of the vena cava can be accomplished using a wedge board (or any hard material) to tilt the body 15 to 30° to the left. The supporting surface should be sufficiently rigid to ensure chest compressions remain effective. Although the empirical evidence supporting these interventions may be limited, they are consistently endorsed by expert panels.
In the event of unsuccessful resuscitation within a 4-minute window, an emergent cesarean section should be considered to optimize fetal outcomes. The gestational age should ideally exceed 20 weeks. If the gestational duration remains uncertain, the cesarean section should be pursued if the fundal height of the uterus reaches or surpasses the level of the umbilicus. The fetus should ideally be delivered within 5 minutes following the maternal cardiac arrest.
- Within the context of pregnancy, hypovolemia and other etiologies of hypotension remain the predominant causes of cardiac arrest.
- Should cardiac arrest occur postpartum, hemorrhage must be promptly considered as a differential, and immediate administration of 1 g intravenous tranexamic acid is recommended.
- In circumstances of hypotension and hemorrhage, it is imperative to administer appropriate fluid or erythrocyte boluses to restore circulatory volume.
- To ensure optimal oxygen delivery, high-flow oxygen therapy (100% FiO2) should be provided to maintain arterial oxygen saturation levels above 95%.
- Given the young age of these patients and the typically short periods of no-flow and low-flow, the early consideration of extracorporeal membrane oxygenation (ECMO) is strongly advised.
References
DeBehnke DJ, Hilander SJ, Dobler DW, Wickman LL, Swart GL. The hemodynamic and arterial blood gas response to asphyxiation: a canine model of pulseless electrical activity. Resuscitation 1995;30:16975.
Safar P, Paradis NA, Weil MH. Asphyxial cardiac arrest. In: Paradis NA, Halperin HR, Kern KB, Wenzel V, Chamberlain DA, editors. Cardiac arrest—the science and practice of resuscitation medicine.
Kitamura T, Kiyohara K, Sakai T, et al. Epidemiology and outcome of adult out-of-hospital cardiac arrest of non-cardiac origin in Osaka: a population-based study. BMJ Open 2014;4:e006462.
Deasy C, Bray J, Smith K, et al. Hanging-associated out-of-hospital cardiac arrests in Melbourne, Australia. Emerg Med 2013;30:3842.
Luna GK, Pavlin EG, Kirkman T, Copass MK, Rice CL. Hemodynamic effects of external cardiac massage in trauma shock. J Trauma 1989;29:1430-3.
Jeffcoach DR, Gallegos JJ, Jesty SA, et al. Use of CPR in hemorrhagic shock, a dog model. J Trauma Acute Care Surg 2016;81:27-33.
Watts S, Smith JE, Gwyther R, Kirkman E. Closed chest compressions reduce survival in an animal model of haemorrhageinduced traumatic cardiac arrest. Resuscitation 2019;140: 37-42.
Endo A, Kojima M, Hong ZJ, Otomo Y, Coimbra R. Open-chest versus closed-chest cardiopulmonary resuscitation in trauma patients with signs of life upon hospital arrival: a retrospective multicenter study. Crit Care 2020;24:541.
Ebo DG, Clarke RC, Mertes PM, et al. Molecular mechanisms and pathophysiology of perioperative hypersensitivity and anaphylaxis: a narrative review. Br J Anaesth 2019;123:e3849.
Wallmuller C, Meron G, Kurkciyan I, et al. Causes of in-hospital cardiac arrest and influence on outcome. Resuscitation 2012;83:120611.
Wang CH, Huang CH, Chang WT, et al. The effects of calcium and sodium bicarbonate on severe hyperkalaemia during cardiopulmonary resuscitation: a retrospective cohort study of adult in-hospital cardiac arrest. Resuscitation 2016;98:10511.
Saarinen S, Nurmi J, Toivio T, et al. Does appropriate treatment of the primary underlying cause of PEA during resuscitation improve patients’ survival? Resuscitation 2012;83:81922.
Mroczek T, Gladki M, Skalski J. Successful resuscitation from accidental hypothermia of 11.8 degrees C: where is the lower bound for human beings? Eur J Cardiothorac Surg 2020;58:10912.
Stephen CR, Dent SJ, Hall KD, Smith WW. Physiologic reactions during profound hypothermia with cardioplegia. Anesthesiology 1961;22:87381.
Frei C, Darocha T, Debaty G, et al. Clinical characteristics and outcomes of witnessed hypothermic cardiac arrest: a systematic review on rescue collapse. Resuscitation 2019;137:418.
Wood S. Interactions between hypoxia and hypothermia. Annu Rev Physiol 1991;53:7185.
Podsiadlo P, Darocha T, Svendsen OS, et al. Outcomes of patients suffering unwitnessed hypothermic cardiac arrest rewarmed with extracorporeal life support: a systematic review. Artif Organs 2020.
