Basic life support (BLS) can be provided by anyone, including laypeople. As shown in Table 1, BLS is an exceptionally effective treatment, with a very low number needed to treat (NNT), indicating high effectiveness. Although BLS is primarily developed for out-of-hospital cardiac arrest (OHCA), it can be used in any setting until advanced cardiac life support (ACLS) can be initiated by healthcare professionals. The purpose of basic cardiopulmonary resuscitation is to keep the person alive until resources and skills to provide ACLS arrive. However, rapid administration of BLS in the event of sudden cardiac arrest may be sufficient to resuscitate the individual, especially if an automatic external defibrillator (AED) is available and used appropriately. According to the Swedish Cardiopulmonary Resuscitation Registry, training laypeople and first responders (such as police, fire brigade, emergency rescue, and security guards) in BLS is key to improving outcomes in OHCA and may be the single strongest factor driving improvement in survival rates.
| Intervention | Included in BLS | NNT to save 1 person | Reference |
|---|---|---|---|
| Early detection of cardiac arrest | Yes | 11 | Berdowski et al |
| Bystander CPR | Yes | 15 | Hasselqvist et al |
| Early defibrillation | Yes, if AED is available | 5 | Kitamura et al |
| Adrenaline (epinephrine) | No | 112 | Perkins et al |
AED = automatic external defibrillator.
The Number Needed to Treat (NNT) is the number of patients you need to treat to save one. If an intervention has an NNT of 10, then 10 people must be treated to save 1.
Number Needed to Treat (NNT)
Basic life support (BLS) includes rapid recognition and treatment of life-threatening conditions or injuries, including cardiac arrest, drowning, trauma, asphyxia and respiratory arrest. BLS can be provided by laymen, EMTs (emergency medical technicians), nurses, paramedics, physicians. BLS is provided until advanced life support (ALS) can be initiated. In regards to cardiac arrest, BLS includes delivering high-quality chest compressions, ventilations and use of an automatic external defibrillator (AED). BLS courses are provided by certified instructors worldwide.
Basic life support (BLS)

1. Safety at the scene
The first step in BLS is to check the scene for safety. BLS can only commence if it is safe for the rescuer, victim and bystanders. Relocate to a safe position if required.
2. Confirm cardiac arrest
In case of a collapse (out-of-hospital or in-hospital) the first task is to determine if a cardiac arrest has occurred. A cardiac arrest is confirmed by the following four examinations:
- Responsiveness: Does the victim respond to stimuli? Shake the victim by the shoulders and ask if the victim is awake.
- Breathing: Open the airway by tilting the head backward and lifting the chin up. Does the person breathe? Look for respiratory signs for 10 seconds.
- Palpation of pulses: carotid, femoral or radial artery.
According to current guidelines, laypeople do not need to perform the 3rd assessment (reliable assessment of pulses requires training and experience). Thus, for laypeople, examinations 1 and 2 are sufficient to confirm a cardiac arrest. All 3 examinations are recommended for medical professionals.
Evaluation of skin color is not necessary to confirm cardiac arrest. Skin color is pale or cyanotic, but this may be difficult to discern depending on the skin tone.
For laypeople, confirming absent or abnormal breathing is sufficient to alert the emergency service and commence CPR.
Agonal breathing before apnea
A cardiac arrest occurs within a minute after cessation of breathing (apnea), regardless of the cause. A person who is not breathing will therefore develop a cardiac arrest. During the first minute after a cardiac arrest, the person may display agonal breathing (irregular, slow, and snoring breaths). One minute after the cardiac arrest, agonal breathing ceases and apnea occurs. Hence, agonal breathing is equated to apnea.
3. Actions after cardiac arrest is confirmed
- Alert — Alert the emergency services (911 in the US, 112 in Europe) in out-of-hospital cardiac arrest. In case of in-hospital cardiac arrest, alert the cardiac arrest team.
- If possible, a bystander is directed to call the emergency services. The phone’s speaker function is activated in order to receive instructions from the emergency dispatcher.
- If possible, send one bystander to find an AED.
- Start — Start CPR (see below).
Early detection of airway obstruction
If the individual has a pulse but lacks breathing, the pharynx should be inspected for foreign bodies causing airway obstruction. If a foreign body is detected in the airway, attempts should be made to extract it manually, alternatively with the Heimlich maneuver.
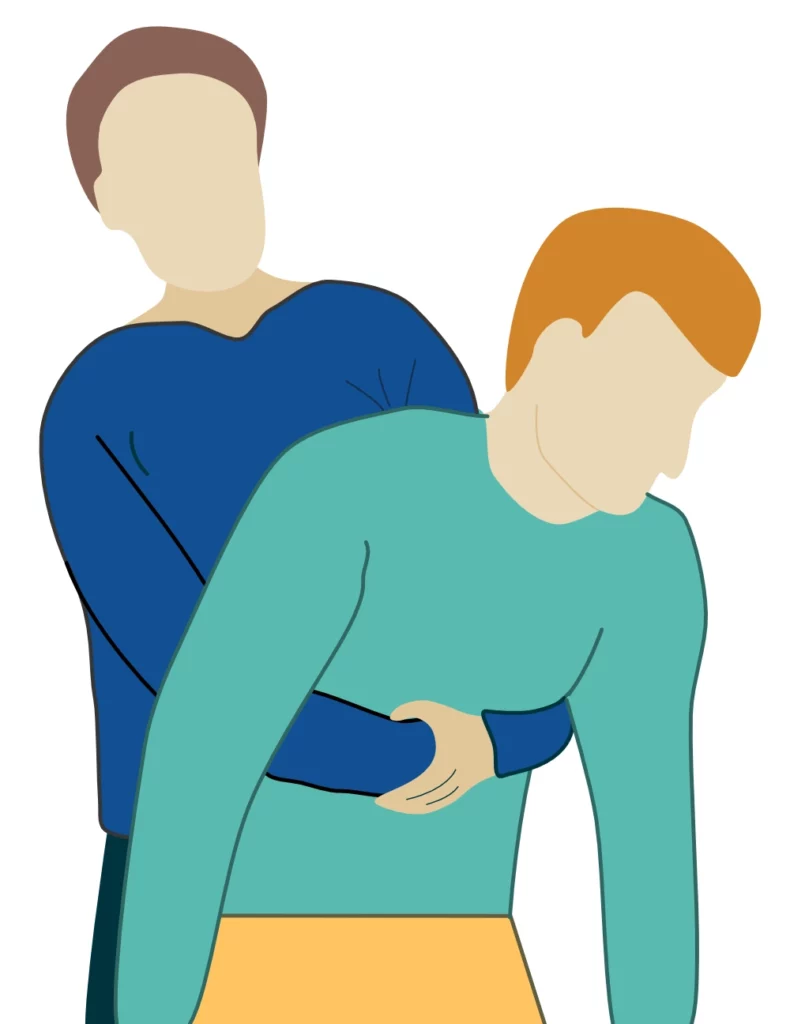
Heimlich maneuver (abdominal thrusts)
The purpose of the Heimlich maneuver is to exert pressure on the bottom of the diaphragm, so that the lugns become compressed and air is forced out of the lungs. This may expell a foreign body lodged in the upper airways. The maneuver is carried out as follows (Figure 3):
- Stand behind the person, and bend the person forward, so that the head falls below the level of the chest.
- Encourage the victim to cough.
- Perform 5 hard back slaps.
- Perform 5 abdominal thrusts by placing your hands around the victim’s abdomen, grasping your hands and pulling them upwards towards you.
Withholding resuscitation (Do Not Attempt CPR, DNACPR)
Approximately 90% of all sudden out-of-hospital cardiac arrests die within 30 days, of which the majority die within the first hours. In a significant proportion of these cases, CPR is started despite the fact that the patient is already dead or certain to die. The justification for initiating CPR is that in the acute setting, several critical parameters (patient preferences, coexisting conditions, no-flow time, low-flow time, etc.), are uncertain or unknown. However, there are indicators that strongly suggest that the individual will die or is already biologically dead.
- Rigor mortis is evidence of death.
- If the cardiac arrest is unwitnessed and the skin is cold, then survival is highly unlikely.
- Survival is 0.5% if a patient meets the following 3 criteria:
- unwitnessed cardiac arrest
- no pre-hospital defibrillation
- no ROSC
The median delay to EMS arrival is about 10 minutes worldwide, which is more than twice the target delay recommended by guidelines (4-6 minutes). Thus, unless high-quality CPR is initiated before EMS arrival, the person is already very seriously injured. Bystander CPR is essential to postpone fatal injuries until EMS arrives and advanced resuscitation can be initiated.
Thumpversion (precordial thump)
Applying a powerful and swift mechanical force to the heart may rarely terminate ventricular tachycardia or ventricular fibrillation. The evidence for thumpversion is very poor, and the intervention should only be used in situations where no other means of defibrillation or cardioversion is available. Thumpversion is performed by thumping the heart or lower sternum with the ulnar aspect of the fist. A powerful thump is required.
If other means of defibrillation or cardioversion (defibrillator, amiodarone, lidocaine, etc) are available, thumpversion should not be performed as it may delay evidence-based CPR.
Basic cardiopulmonary resuscitation (CPR)
Anyone can provide basic CPR.
Basic cardiopulmonary resuscitation can be provided by medical professionals, police, fire brigade, emergency services, and laypeople. Basic CPR includes chest compressions and ventilation. Increasingly, AEDs are being used in basic CPR. This is possible because AEDs are easy to use, and available in an increasing number of public places. In some countries, the emergency dispatcher is able to use geolocation services in smartphones to dispatch volunteers, including sending them for an AED. Hence, it is becoming increasingly common for the EMS to arrive at the scene with a defibrillator already connected to the victim.
Basic CPR includes four components:
- Compressions – Perform chest compressions.
- Airway – Establish a free airway.
- Breathing — Ventilate by providing rescue breaths.
- AED – Connect and use AED if available.
Chest compressions
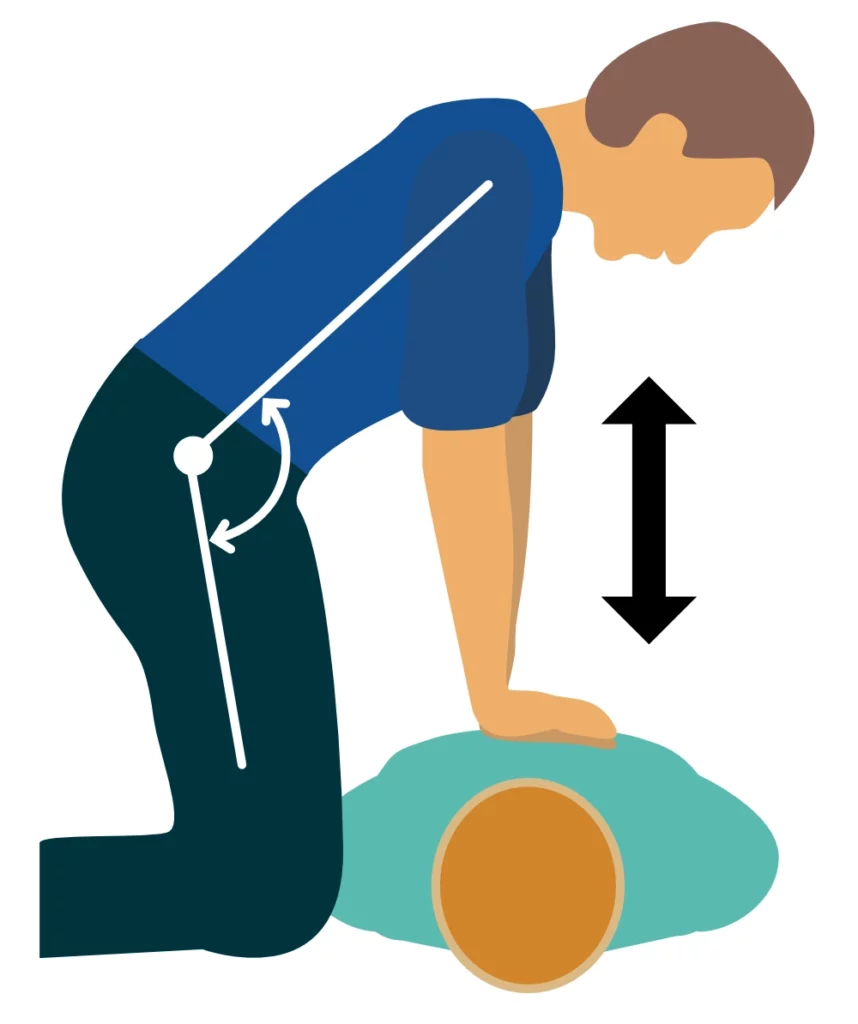
- Place one hand on the lower half of the sternum, and place the second hand on the top of the first hand.
- Push down the chest with straight arms. Do not bend the elbow. Compression work should be carried out with the back and torso muscles, allowing more effective compressions
- The speed is 100 to 120 compressions per minute.
- The sternum should be pressed down 5-6 cm.
- After each compression, the sternum should be discharged quickly and completely.
Compression-Ventilation ratio
The compression-ventilation ratio is the ratio of compressions to ventilations. The ratios in various situations are as follows:
- Adults: 30:2 (30 compressions followed by 2 ventilations).
- Adults, if the rescuer is uncertain about performing ventilation: only compressions (uninterrupted), no ventilation.
- Infants and children with one rescuer: 30:2.
- Infants and children with two rescuers: 15:2.
Unless it is possible to defibrillate immediately, chest compressions are the single most important measure to resuscitate a victim from cardiac arrest. High-quality compressions can generate cardiac output equal to 20–25% of normal circulation (assuming that the valves are functioning normally).
Mechanisms driving cardiac output
The chapter The Physiology of Cardiopulmonary Resuscitation delves into the physiological mechanisms behind how chest compressions generate cardiac output. In summary, the act of compressing and decompressing the chest causes variations in intrathoracic pressure. During the decompression phase, the low pressure in the right atrium allows blood to flow passively to the right atrium and the right ventricle. Conversely, during the compression phase, the entire intrathoracic pressure increases, leading to increased pressure in all tissues and chambers. Provided that the valves function normally, the blood is ejected in an anterograde direction, toward the aorta and thus the coronary and cerebral arteries. The heart can only be restarted if coronary blood flow is sufficient. The coronary perfusion pressure (CPP) must be at least 15 mmHg to elicit cardiac electrical activity, which is a prerequisite for cardiac mechanical function and achieving ROSC (return of spontaneous circulation). The greater the coronary perfusion pressure, the more likely it is to induce electrical activity and succeed in defibrillating ventricular tachycardia or ventricular fibrillation (Ewy et al). Interrupting compressions have an immediate and detrimental impact on coronary perfusion pressure, which requires many valuable seconds to rebuild.
Compressions-only CPR (hands-only CPR)
CPR with compressions only (hands-only CPR, compression-only CPR) is perhaps equivalent to standard CPR in out-of-hospital cardiac arrest (Jerkemean et al, Riva et al). Therefore, this can be recommended if the rescuer is uncertain about performing ventilation (rescue breaths).
Compression fraction
It is critical to minimize the number and length of interruptions in chest compressions. Interruptions are allowed for ventilation, rhythm control, defibrillation.
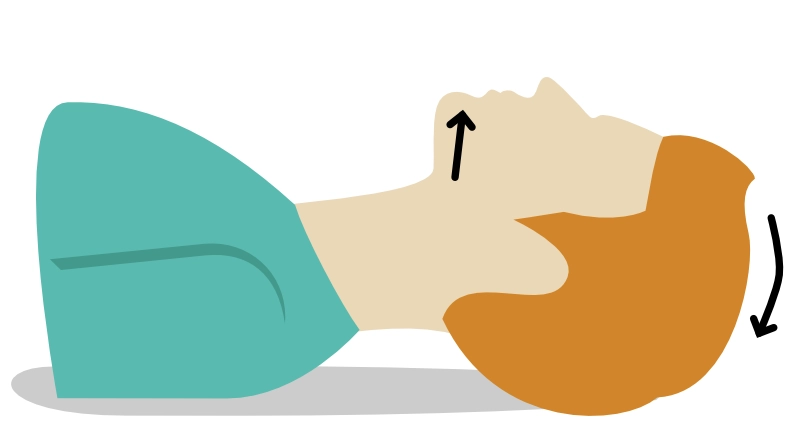
Airway
A free airway is established by lifting the chin and tilting the head backward. This is a very effective method, although repositioning may be required if rescue breaths are met by high resistance.
Suffocation
- Explore the oral cavity and pharynx for foreign bodies and loose dental implants.
- Foreign body obstruction should be suspected if the victim was unable to speak before the cardiac arrest, especially if it occurred during food intake.
- If the victim has not yet collapsed and shows signs of suffocation, the victim should be encouraged to cough. If coughing does not work, the rescuer should perform the Heimlich maneuver, starting with 5 hard back slaps. Repeat the Heimlich maneuver until the obstruction is expelled, or the victim loses consciousness, upon which CPR is initiated.
Ventilation
Mouth-to-mouth ventilation is the standard procedure for out-of-hospital cardiac arrest. Mouth-to-nose ventilation is only used if mouth-to-mouth is not feasible (e.g. due to trauma or difficulties sealing the mouth).
Performing rescue breaths
- Open the airways using chin lift and head tilt.
- Closes the victim’s nose by pinching it.
- Enclose the victim’s mouth with your mouth and provide 2 rescue breaths.
Each rescue breath is given over 1 second. The rescuer takes a normal breath before delivering a rescue breath. Avoid deep breaths before providing rescue breaths. Excessive ventilation causes an unnecessary increase in intrathoracic pressure and subsequently diminishes venous return, coronary perfusion pressure and cardiac output. Unfortunately, excessive ventilation is common in ACLS (Aufderheide et al).
Early defibrillation by first responders
First responders include police, fire brigade, emergency services, security guards and laypeople. If a first responder is first at the scene and performs defibrillation, survival is 67%, as compared with 43% if the defibrillation is performed by the EMS. This difference reflects the importance of early defibrillation (Pollack et al). A first responder can only defibrillate if a defibrillator (typically semi-automatic or fully-automatic) is available in a public place or in a vehicle (police car, fire truck, etc.).
- If two rescuers are present, one performs CPR while the other connects the AED.
- The AED is connected, started and instructions are followed.
- Avoid touching the victim during analysis or defibrillation.
- Start compressions immediately after defibrillation.
Continue compressions when the AED is charging. A fully-automatic defibrillator (i.e. an AED) automatically defibrillates, after instructing the rescuers to stand back, when possible. A semi-automatic defibrillator indicates when an electric shock should be delivered.
Publicly available defibrillators are very safe, effective and should be used whenever possible.
References
Berdowski J, Beekhuis F, Zwinderman AH, Tijssen JG, Koster RW. Importance of the first link: description and recognition of an out-of-hospital cardiac arrest in an emergency call. Circulation 2009; 119:2096-2102.
Hasselqvist-Ax I, Riva G, Herlitz J, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2015; 372:2307-2315.
Kitamura T, Kiyohara K, Sakai T, et al. Public-access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med 2016; 375:1649-1659.
Ewy G.A. Cardiocerebral and cardiopulmonary resuscitation – 2017 update. Acute Med Surg. 2017; 4:227 —234. 29123868
Pollack R.A, Brown S.P, Rea T, et al. Impact of bystander automated external defibrillator use on survival and functional outcomes in shockable observed public cardiac arrests. Circulation. 2018; 137:2104—2113. 29483086
Aufderheide TP, Sigurdsson G, Pirrallo RG, Yannopoulos D, McKnite S, von Briesen C, Sparks CW, Conrad CJ, Provo TA, Lurie KG. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960–1965. doi: 10.1161/01.CIR.0000126594.79136.61
