Pacemaker malfunction, troubleshooting and ECG
Conventional surface ECG can reveal the following types of pacemaker dysfunction:
- Failure to capture (FTC), which means that the pacemaker stimulations do not result in myocardial activation.
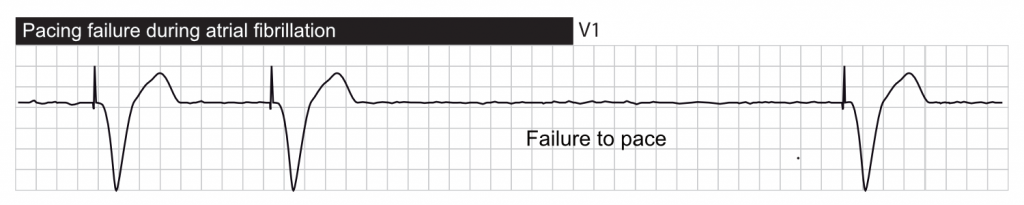
- Failure to pace (FTP), which means that the pacemaker does not stimulate as expected.
- Oversensing, which means that the pacemaker senses signals that are not true P-waves or R-waves. Sensing of such signals normally inhibits the pacemaker. Oversensing may lead to underpacing.
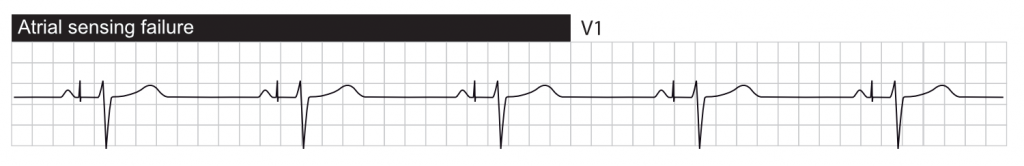
- Failure to sense (undersensing), which means that it fails to sense true P-waves or R-waves. Undersensing may lead to overpacing.
- Failure to rate adjust, which means that the pacemaker fails to adjust its rate according to haemodynamic needs. This is only relevant in rate responsive pacemakers.
These failures typically result in missing stimulation artifacts, misplaced stimulation artifacts, irregular pacing, etc. Most cases of malfunction are associated with the electronics in the pulse generator or dislodgement or fracture of the leads. External causes are less common and include electrolyte disorders, metabolic disorders, hypoxemia, antiarrhythmic drugs, or electromagnetic disturbance caused by other machines/devices.
Below follows ECG tracings demonstrating each type of failure.
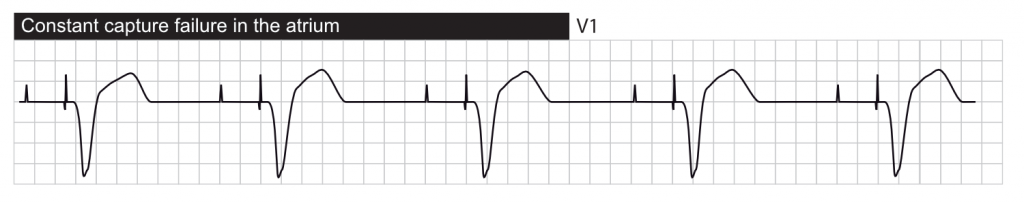
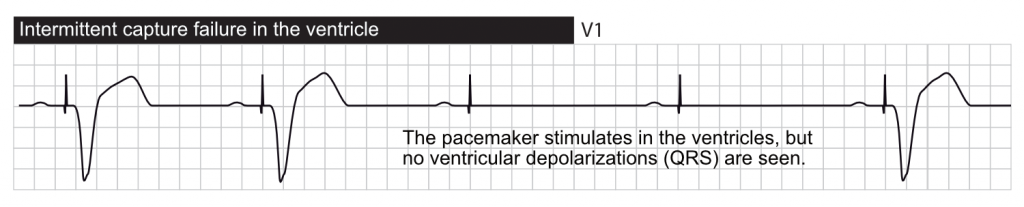
Failure to capture
Definition: pacing does not result in myocardial activation.
Two types of failure to capture should be distinguished:
- Genuine failure to capture occurs when a stimulus that is expected to result in activation fails to do so. This may be due to insufficient stimulus energy, or lead dislodgement/fracture.
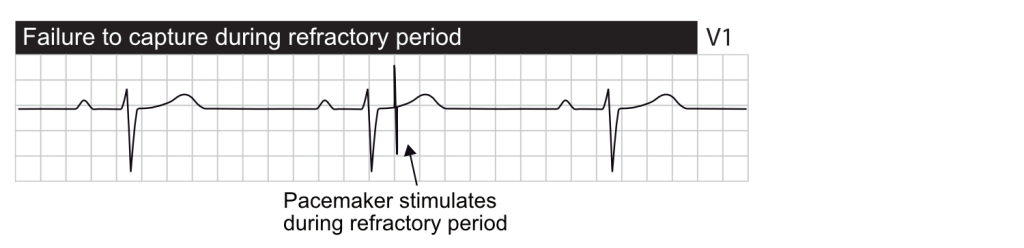
- Functional failure to capture occurs when a stimulus is delivered during the myocardial refractory period. A stimulus delivered during the refractory period should not result in activation because the myocardium is refractory.
The most common cause of failure to capture is insufficient stimulus energy. Modern pacemakers have built-in functions to calibrate the stimulus amplitude and width according to myocardial excitability. This is done by repeatedly stimulating with gradually decreasing amounts of energy until the stimulus no longer yields an activation. The pacemaker is then set to the minimum energy needed to activate myocardium (a safety margin is often used). Most pacemakers perform such calibrations several times daily, and they include a backup algorithm that delivers a stimulus when failure to capture is confirmed.
Oversensing
Oversensing occurs when the pacemaker detects electrical activity that it incorrectly interprets as atrial (P-wave) or ventricular activity (R-wave). The signals causing oversensing may not be visible on surface ECG.
Oversensing may also occur when electrical events in one chamber is sensed by the lead in the other chamber, resulting in inappropriate inhibition of the pacemaker in the latter chamber. This type of oversensing is referred to as pacemaker crosstalk.
Oversensing may also occur when the ventricular lead interprets the T-wave as an R-wave.
In DDD pacing, atrial oversensing leads to rapid ventricular pacing.
In DDI pacing, atrial oversensing leads to ventricular underpacing.
Undersensing
Undersensing occurs when the pacemaker fails to detect cardiac activity. This may be due to lead dislodgement, lead fracture or inadequate myocardial contact. It may also be due to the low amplitude (voltage) of the potentials generated by activated myocardium.
Functional undersensing occurs when the pacemaker does not sense intrinsic activity during the period when sensing is disabled. This is an appropriate form of undersensing, and was discussed previously (refer to PVARP).
Undersensing can lead to overpacing, because the pacemaker does not sense ongoing activity. Signs of overpacing should always lead to suspicion of undersensing.
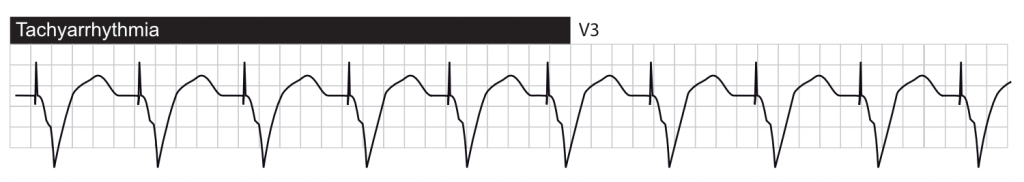
Tachyarrhythmias
If ventricular pacing is triggered by atrial activity, then tachyarrhythmias may occur in the following situations:
- A supraventricular tachyarrhythmia (e.g atrial fibrillation) can be transmitted to the ventricles.
- If the ventricular impulse manages to travel in retrograde direction back to the atria, via the bundle of His, then it may trigger another ventricular stimulation. This may result in an endless loop tachycardia, also called pacemaker mediated tachyarrhythmia / tachycardia (PMT). PMT may be terminated by placing a magnet on the pulse generator. Modern pacemakers often include algorithms that detect and terminate PMT.
- When oversensing in the atrium, ventricular pacing may increase inappropriately.
Recall from the previous discussion that PVARP, mode switch and upper pacing limit are means for preventing these tachyarrhythmias. PVARP means that the atrial lead is refractory for a certain time period after each ventricular stimulation. Mode switch means that the pacemaker inactivates the trigger function during supraventricular tachyarrhythmias. Also note that tachyarrhythmias mediated by the pacemaker can not exceed the upper pacing limit of the pacemaker, which is usually set to 160 beats/min.
Other tachyarrhythmias associated with pacemaker
Rate responsiveness
The sensor enabling rate responsiveness may misinterpret signals and assume that the person is physically active, and thus increase the ventricular rate. For example, sensors that record movements (accelerometer) may misinterpret external vibrations as physical activity.
Runaway pacemaker
Runaway pacemaker is a potentially life-threatening condition in which the pacemaker fires >200 times per minute, which may degenerate into ventricular fibrillation. The most common cause is battery failure or external damage. Placing a magnet on the pulse generator may resolve the arrhythmia, but more aggressive measures may be necessary.

