Introduction to Coronary Artery Disease (Ischemic Heart Disease) & Use of ECG
Coronary artery disease (ischemic heart disease)
Coronary artery disease, which is synonymous with ischemic heart disease, is the most common form of cardiovascular disease. It has been the number one killer in Western and high-income countries for more than half a century, causing approximately 20% of all deaths in these regions. Mortality rates and case fatality in coronary artery disease peaked in the 1970s and have declined steadily ever since. The marked decline in death rates and case fatality is most likely explained by successful primary preventive strategies, such as reduced smoking rates, aggressive lowering of blood lipids with statins and sophisticated treatments for hypertension. However, coronary artery disease remains the number one killer in most regions worldwide (Tsao et al.).
The New England Journal of Medicine, 1812. Remarks on Angina Pectoris by John Warren
The remarkable facts, that the paroxysm, or indeed the disease itself, is excited more especially upon walking up hill, and after a meal; that thus excited, it is accompanied with a sensation, which threatens instant death if the motion is persisted in; and, that on stopping, the distress immediately abates, or altogether subsides; have . . . formed a constituent part of the character of Angina Pectoris.
Atherosclerosis: the cause of coronary artery disease
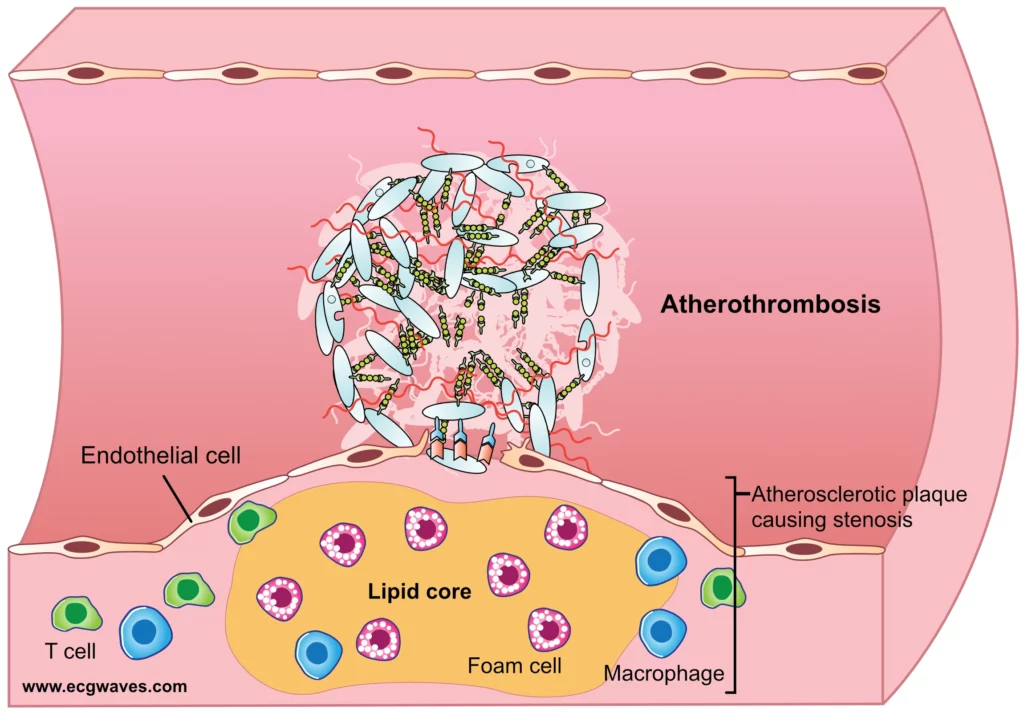
The underlying cause is atherosclerosis, which is a chronic inflammatory disease of the arteries. It has become increasingly clear in the past few decades that atherosclerosis is not caused by the passive deposition of lipids into the coronary artery walls; indeed, atherosclerosis is a disease in which the immune system elicits an active inflammation within the artery wall and lipids (particularly LDL cholesterol) plays a key role. As the inflammation and deposition of lipids progress, an atherosclerotic plaque forms in the wall of the artery. Such atherosclerotic plaques start building up early in childhood and by middle age, most persons have some degree of atherosclerosis in the coronary arteries. Advanced atherosclerotic plaques contain inflammatory cells, smooth muscle cells, extracellular matrix, lipids and acellular debris. The interplay between inflammation and risk factors (smoking, hypertension, hyperlipidemia, diabetes, etc) modifies the progression rate in the atherosclerotic plaque. The more inflammation and more risk factors, the more aggressive atherosclerosis. Moreover, inflammation and risk factors also modify the risk of destabilization of the plaque; atherosclerotic plaques are vulnerable and may disrupt, which may ultimately lead to death (Stone, Libby et al.).
As the atherosclerotic plaque increases in size, it bulges into the artery lumen and causes stenosis (reduction of the artery lumen). The reduction of the artery lumen causes limitations to the blood flow. This may cause symptoms in situations with increased cardiac workload (physical exercise) because the increased workload leads to increased oxygen demand but the stenosis limits the volume that can be delivered to the heart muscle supplied by the atherosclerotic artery. Whenever oxygen demand exceeds oxygen (blood) delivery ischemia occurs and this manifests with chest discomfort referred to as angina pectoris. If the physical activity ceases, the myocardial oxygen demand will gradually decline and the symptoms disappear within minutes. Stable coronary plaques cause symptoms at the same level of myocardial workload and the symptoms disappear within minutes after stopping the activity. The greater the stenosis, the lower the level of myocardial workload required to elicit ischemia and symptoms.
Angina pectoris: the hallmark of coronary artery disease
Angina pectoris is the cardinal symptom of coronary artery disease. It occurs when the myocardium becomes ischemic. It is typically described as a diffuse pain over the anterior chest wall. The pain may be experienced as a pressure, cramp or crushing sensation. The pain may radiate to either arm, neck, back or shoulder. Angina pectoris is often accompanied by shortness of breath (dyspnea). If these symptoms are stable over time, then the condition is classified as stable angina pectoris and this implies that the coronary artery disease is significant but stable. Patients with stable angina pectoris only experience angina (chest pain) in situations with increased myocardial workload, and symptoms subside when the workload returns to normal. The most typical scenario is angina pectoris provoked by physical exercise or mental stress. Both these scenarios increase heart rate and workload which subsequently causes myocardial ischemia. Importantly, in stable angina pectoris, the symptoms subside within minutes after resting or after administration of nitroglycerin. Also, the level of physical activity that elicits angina must be stable during the past few weeks. Please refer to Approach to Patients with Chest Pain for details regarding the evaluation of chest pain patients.
The size of coronary plaques tends to increase with time. This leads to increased stenosis (the arterial lumen becomes more narrow) and thus more pronounced symptoms (i.e symptoms at lower myocardial workloads). Notably, research conducted in the past few years has shown that intensive statin treatment may slow, inhibit or even reverse this progression (The JUPITER Study, Ridker et al).
Atherosclerotic plaques are frail: damage causes acute coronary syndromes and myocardial infarction
The most serious scenario emerges if the atherosclerotic plaque is damaged, either by rupturing or by erosion of the endothelium covering the plaque. This is generally the result of intensive inflammation within the plaque. As mentioned above, the plaque houses inflammatory (immune) cells that maintain a chronic inflammation within the plaque. Chronic inflammation destabilizes the plaque and ultimately results in a rupture or erosion. A damaged plaque exposes thrombogenic substances located within the artery wall (e.g collagen). Such thrombogenic substances will activate thrombocytes and coagulation factors that pass by and this leads to the formation of a thrombus (atherothrombosis; formation of a thrombus within an artery). This process only takes a few minutes, or even less. The thrombus occludes the artery either completely or partially. In either case, the sudden reduction in arterial blood flow will lead to myocardial ischemia. This type of ischemia is typically very severe and causes persisting chest discomfort which is not alleviated by rest and nitroglycerin barely mitigates the pain. This scenario, in which a ruptured/eroded atherosclerotic plaque causes atherothrombosis with ensuing severe myocardial ischemia, is referred to as an acute coronary syndrome. Please refer to Figure 1.
Acute coronary syndrome and myocardial infarction
As mentioned above, an acute coronary syndrome occurs when coronary blood flow is reduced suddenly and severely due to atherothrombosis. The myocardial muscle supplied by the occluded artery will immediately become ischemic. If blood flow is not restored rapidly, the ischemic area will undergo infarction (necrosis) which leads to irreversible cell death. The infarction will commence in the most ischemic area and from there it will gradually expand. If the artery is completely occluded (i.e no flow through the artery) all ischemic myocardium will be dead within 2 to 12 hours. The size of the ischemic/necrotic area correlates strongly with the risk of heart failure, malignant ventricular arrhythmias, and other complications. The risk of malignant ventricular arrhythmias (ventricular tachycardia, ventricular fibrillation) is highest in the hyperacute phase (the first hour). Because most patients delay before seeking medical attention, those who die from acute myocardial infarction tend to do so outside of the hospital. This also means that the mere arrival to hospital indicates a good prognosis.
It should be noted that the natural course outlined above – i.e the progression from stable coronary artery disease to acute myocardial infarction – is not universal. The majority of patients with coronary artery disease never develop acute coronary syndromes. On the other hand, some develop acute myocardial infarction as their first sign of coronary artery disease. Moreover, the vast majority of middle-aged and older individuals do have some degree of atherosclerosis but only a minority will progress to symptomatic heart disease (more about this below).
Risk factors of coronary artery disease and acute myocardial infarction
Risk factors of coronary artery disease are some of the most intensively researched areas of medicine. Thousands of studies, ranging from genomics to nationwide epidemiological studies, have elucidated risk factors of coronary artery disease. The INTERHEART study deserves special mention because it was conducted in 52 countries, including all continents. The INTERHEART study showed that more than 90% of the total risk of developing acute myocardial infarction was explained by nine simple modifiable risk factors. This was true for men and women in all 52 countries. It follows that the vast majority of all myocardial infarctions may be prevented by targeting these risk factors. The INTERHEART study brought rather spectacular news, as it was previously believed that only 50% of the risk was modifiable. Virtually all studies have shown that the most important risk factors are high blood lipids (hyperlipidemia), smoking, hypertension, and diabetes. Other significant risk factors are abdominal obesity, psychosocial stress, low levels of physical activity, low intake of fruits and vegetables, etc. Importantly, hyperlipidemia (sometimes referred to as dyslipidemia) and smoking constitute 66% of the risk of myocardial infarction.
Table 1: Risk factors for acute myocardial infarction (The INTERHEART Study)
| RISK FACTOR | RELATIVE RISK |
| High blood lipids | 3.25 |
| Current smoking | 2.87 |
| Diabetes | 2.37 |
| Hypertension | 1.91 |
| Abdominal obesity | 1.62 |
| Psychosocial stress | 2.67 |
| Daily consumption of vegetables and fruit | 0.7 |
| Physical exercise | 0.86 |
| Alcohol intake | 0.91 |
How to interpret the numbers: e.g., high blood lipids are associated with a relative risk of 3.25, which implies that having high blood lipids, as compared with having normal blood lipids, is associated with 3.25 times as great a risk of acute myocardial infarction.
High blood lipids (hyperlipidemia) deserve special mention since the condition is very common and easy to treat. As noted in Table 1 hyperlipidemia is associated with 3.25 times as great a risk of acute myocardial infarction. Actually, all levels of blood lipids are associated with the risk of myocardial infarction. The lower the lipid levels, the lower the risk of myocardial infarction. Note that blood lipids are actually transported in lipoprotein complexes, which are large spheric complexes consisting of lipids and proteins. Lipoproteins are measured to evaluate blood lipid levels. There are numerous types of lipoproteins, such as LDL cholesterol, HDL cholesterol, VLDL cholesterol, etc. LDL (low-density lipoprotein) cholesterol is the most important lipoprotein; the higher the LDL cholesterol, the more aggressive the atherosclerotic process.
Body Mass Index (BMI) is not as strongly associated with the risk of acute myocardial infarction, as compared with abdominal obesity. Psychosocial stress (economic stress, workplace stress, depression, domestic stress) are comparable to hypertension and abdominal obesity. Smokers have 2.87 times as great a risk of myocardial infarction, as compared with non-smokers. Smoking one to five cigarettes per day increases the risk of infarction by 40%. Smoking 20 cigarettes per day increase the risk by 400% (i.e. 4 times as great a risk as compared with non-smokers).
To conclude, the vast majority of myocardial infarctions may be prevented. More than 90% of the risk is explained by modifiable risk factors. Virtually all risk factors may be treated with evidence-based, cheap and readily available medications.
The ECG in ischemic heart disease
The ECG is an invaluable tool in acute and chronic myocardial ischemia. Optimal use of the ECG will provide information on diagnosis, prognosis and appropriate treatments. In acute ischemia, the ECG will also provide information on the extension, localization and time course of the ischemia. This is rather remarkable given that an ECG recording costs approximately $10.
Because ischemia primarily affects myocardial repolarization, it will cause changes in the ST-segment and T-wave (collectively referred to as ST-T changes). The classical ST-T changes are ST-segment depression, ST-segment elevation, T-wave inversion (i.e. negative T-waves), and flattening of the T-waves or T-waves with increased amplitude. Note that ST depressions, ST elevations and T-wave inversions are absolutely not specific to myocardial ischemia. However, in the setting of chest discomfort, these ST-T changes strongly suggest myocardial ischemia. Careful examination of the morphology of the ST-T changes usually leads to a definitive diagnosis. Also, note that the ECG may show one or several of these ST-T changes. The localization, time course and extent of ischemia will govern exactly which ECG changes that occur. ECG changes seen in the early phase of ischemia differ from those seen in the late phases.
Infarction, on the other hand, affects myocardial depolarization (frankly, dead myocardial cells do not depolarize) which affects the QRS complex. The most characteristic finding is abnormally large Q waves (referred to as pathological Q waves). Other common findings are reduced R-wave amplitude (due to loss of viable myocardium) and fragmented or notched QRS complexes.
ECG changes in myocardial ischemia and infarction will be discussed in great detail.
Use of ECG to classify stages of coronary artery disease
The ECG is utilized in all phases of coronary artery disease to classify the condition. Notably, the ECG is used to guide the management of patients with acute coronary syndromes. ECG characteristics (ST-T changes, QRS changes, criteria, etc) of ischemia and infarction will be discussed in great detail in the subsequent chapters. For now, we will only note the following:
- Stable coronary artery disease (stable angina pectoris) does not cause any ST-T changes at rest. To reveal ischemic ST-T changes the patient must undergo exercise stress (ECG) testing. The purpose of the exercise stress test is to provoke ischemia (ST-T changes) while performing the ECG.
- If a person with stable coronary artery disease displays QRS changes (pathological Q-waves, fragmented QRS, reduced R-wave amplitude), it strongly suggests previous myocardial infarction.
- In the case of acute coronary syndrome, the ECG is used to classify the syndrome into STE-ACS and NSTE-ACS. This subdivision is fundamental because it affects management and immediate treatment.
- STE-ACS (ST Elevation Acute Coronary Syndrome): acute coronary syndromes with ST elevations on ECG are classified as STE-ACS. Virtually all these patients will develop myocardial infarction, which is then classified as STEMI (ST Elevation Myocardial Infarction).
- NSTE-ACS (Non-ST Elevation Acute Coronary Syndrome): acute coronary syndromes without ST elevations on ECG are classified as NSTE-ACS. If the patient develops myocardial infarction, then the condition is classified as NSTEMI (Non-ST Elevation Myocardial Infarction). If the patient does not develop infarction, then the condition is classified as unstable angina.
The perfect storm scenario
Although the majority of adults in high-income countries have some degree of atherosclerosis, the annual incidence of acute coronary syndromes is only 0.2 to 1.0% in individuals aged 40 years or older. Hence, the annual risk of developing an acute coronary syndrome is very small. Studies show that the majority of plaque damages (ruptures, erosions) do not lead to acute coronary syndromes, even though they cause thrombosis. Interestingly, plaque damage and ensuing thrombosis appear to be rather common events that mostly pass asymptomatic. Moreover, studies show that these asymptomatic events appear to be a mechanism driving plaque progression (increase in plaque volume). Thus, acute coronary syndromes are fairly uncommon consequences of plaque damage.
A large body of science indicates that acute coronary syndromes only occur if the plaque damages coincide with a moment in which pro-thrombogenic factors outweigh pro-thrombolytic factors in the blood. Examples of such factors are thrombocyte levels, thrombocyte reactivity, availability of fibrinogen, degree of systemic inflammation, availability of coagulation factors, etc. These factors vary over the course of the day and they are also modified by external factors such as stress, food, medications, toxins (smoking, air pollution), etc. Studies show that there is a circadian variation in the activity of the coagulation factors and thrombocytes, such that it is higher in the morning hours. It is believed that this explains why the incidence of acute myocardial infarction is higher in the morning hours. To conclude, the balance between pro-thrombogenic and pro-thrombolytic factors varies from one minute to another and they determine whether plaque rupture/erosion will lead to occlusive atherothrombosis.
The morphology of atherosclerotic plaques appears to be dynamic. Studies using IVUS (intravascular ultrasound) show that the majority of high-risk plaques (large plaques with thin fibrous caps) tend to revert to more stable plaques over time (within one year) and vice versa (stable plaques tend to progress to more unstable forms). IVUS studies also show that high-intensity statin therapy is very likely to inhibit plaque progression, and even revert it.
One may wonder whether the degree of stenosis is a risk factor for acute coronary syndromes. Some studies have shown that large plaques are associated with a greater risk of acute coronary syndromes, while other studies have not been able to confirm this. Other studies show that the majority of acute coronary syndromes occur in plaques with moderate stenosis. Thus, this question remains unanswered. It is, however, very clear that the level of inflammation in the plaque is critical. The greater the inflammation (regardless of plaque volume) the greater the risk of rupture and development of acute coronary syndrome.
Of all acute coronary syndromes, plaque ruptures cause 60–75%, whereas plaque erosion causes 35–40%. The level of atherosclerosis varies greatly among people who develop acute coronary syndromes. Approximately 5–10% have left main coronary artery (LMCA) disease (i.e. stenosis); 20% have one-vessel disease; 30% have two-vessel disease and 40% have three-vessel disease.
References
Arbab-Zadeh et al: Acute Coronary Events; Circulation 2012
Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics—2022 Update: A Report From the American Heart Association. Circulation 2022; 145: e153–639.
Stone PH, Libby P, Boden WE. Fundamental Pathobiology of Coronary Atherosclerosis and Clinical Implications for Chronic Ischemic Heart Disease Management—The Plaque Hypothesis: A Narrative Review. JAMA Cardiol 2023; 8: 192.

